Introduction
In today’s world, where information has become a tradable commodity, it is mandatory for healthcare organizations and associates to safeguard data provided by patients by becoming HIPAA compliant. As more and more healthcare service providers began to rely on electronic health records (EHR) to create a patient database, data breaches seem to have been taking an upward trend in the last 10 years.
The US Department of Health and Human Services’ (HHS) Office for Civil Rights (OCR) has reported 4,419 data breaches of over 500 records between the years 2009 and 2021. To prevent the disclosure of sensitive patient health information without the patient’s consent or knowledge, a federal law called the Health Insurance Portability and Accountability Act of 1996 (HIPAA) was enforced.
What is HIPAA compliance and its associated rules?
HIPAA created national standards and regulations for Protected Health Information (PHI). Various business practices and covered entities enforce PHI security by being HIPAA compliant, thereby keeping patients’ medical data private. HIPAA compliance, regulated by HHS and enforced by OCR, is a process in which covered entities and business associates comply with HIPAA safeguards and rules to avoid misuse of sensitive patient data. There are two types of organizations that need to be HIPAA compliant:
-Covered Entities: This category includes any organization that has been approved to collect, create or transmit PHI for transactions including claims, benefit eligibility inquiries, and referral authorization requests. Covered entities regulated by HIPAA are healthcare providers, health insurance companies, health maintenance organizations, and healthcare clearing houses.
-Business Associates: To process claims, analyze data, and carry out billing, HIPAA recognizes organizations (other than the covered entity’s workforce) to use the PHI. HIPAA compliant business associates include EHR platforms, billing companies, third-party consultants, practice management companies, accountancy firms, IT service companies, physical or cloud storage companies etc.
Covered entities and business associates have to follow certain rules to stay HIPAA compliant, which are described below;
HIPAA Privacy Rule
This rule contains standards to safeguard the use and prevent disclosure of PHI. The Privacy Rule allows safe exchange of patient information for better healthcare provision, while ensuring that the data is protected. Therefore, the sensitive patient information is only accessible to the covered entities as long as they remain HIPAA compliant. Only covered entities are supposed to follow HIPAA Privacy Rule. The standards of HIPAA Privacy rule include patients’ rights to access PHI, health care providers’ rights to deny access to PHI, the contents of Use and Disclosure HIPAA release forms and Notices of Privacy Practices.
HIPAA Security Rule
The security rule establishes national security standards that covered entities must follow to safeguard patient’s e-PHI. Any health information that is electronically stored or transmitted, is protected under the HIPAA Security Rule, which allows covered entities to use new technologies for advanced patient care while maintaining the safety of e-PHI through physical administration and technical safeguards.
HIPAA Breach Notification Rule
In case there is a data breach of PHI or e-PHI, covered entities and business associates have to follow a specific set of standards to report all breaches. Covered entities must notify affected individuals through first-class mail or e-mail, or alert the media outlets in case there is a breach affecting more than 500 residents. If the breach occurs by a business associate, they must notify the covered entity, which takes further action.
HIPAA Omnibus Rule
A final rule, implementing a number of provisions of the Health Information Technology for Economic and Clinical Health (HITECH) Act, enacted as part of the American Recovery and Reinvestment Act of 2009, was established by the HHS and OCR in 2013. Under this rule, business associates are obligated to be HIPAA compliant. In addition, the Omnibus Rule modified the breach notification standard, privacy and enforcement rules, changed access to and disclosure of PHI and addressed obligations under the Generic Information Nondiscrimination Act, 2008 (GINA).
Why do healthcare providers need to be HIPAA compliant?
Most healthcare providers are shifting from paper records to digital operations, which establishes the need for them to be HIPAA compliant. EHR, computerized physician order entry (CPOE), automated patient management systems, and other digital records have increased the security risks faced by the healthcare industry. HIPAA laws allow the healthcare organizations to restrict access to the sensitive health information and function as HIPAA compliant organizations by ensuring safe storage and transmission of data.
HIPPA rules protect patients from potential identity theft and prevent criminals from seeking healthcare under false pretense. Moreover, being associated with HIPAA compliant organizations puts the patients at ease that their health records are protected and easily accessible for them. Thus, HIPAA compliant healthcare providers ensure that patients do not have to worry about financial implications of data breaches, thereby building trust and confidence for delivery of healthcare services.

Common HIPAA violations
Most data breaches occur due to common HIPAA violations. These violations can persist for months and even years before they are discovered. Hence, it becomes crucial to know about them, so that a medical practice can be safeguarded from these violations. The common HIPAA violations are discussed below;
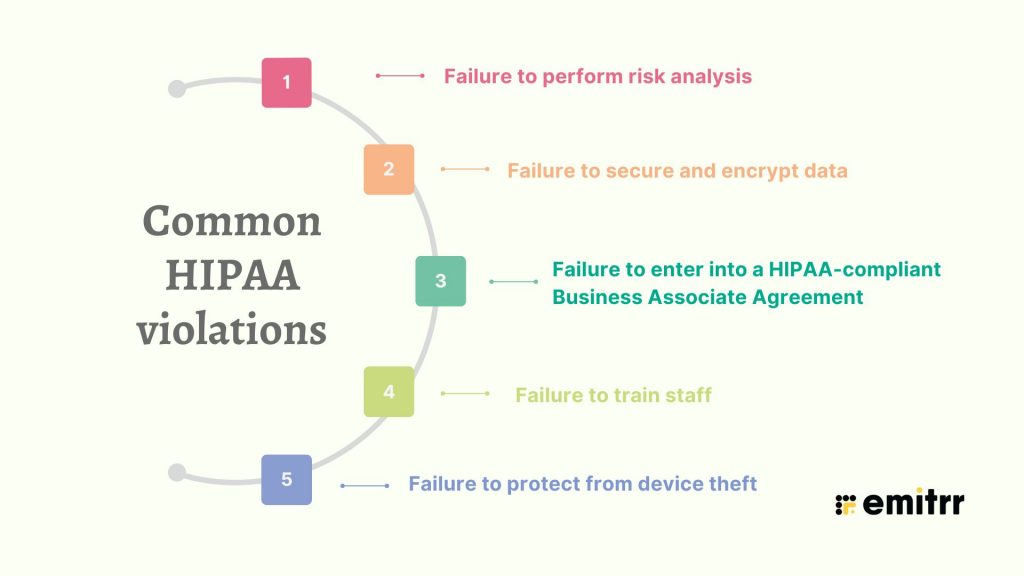
Failure to perform risk analysis
To determine the vulnerability of an organization, a risk analysis of PHI should be performed at regular intervals. Incorporating external vulnerability scanning as part of this process helps identify weaknesses in networks or systems that might be exploited by attackers. In case if risk analysis is not carried out, the organization remains susceptible to threats.
Failure to secure and encrypt data
When organizations fail to protect data due to human error, it can lead to data breach. Leaving records unattended, sharing unsecured patient information and downloading records onto unsecured devices are counted as HIPAA violations. Violation of HIPAA laws also occurs when medical practitioners fail to encrypt data.
Failure to enter into a HIPAA-compliant Business Associate Agreement
By associating with a business channel, a healthcare provider has to provide them access to PHI. If the agreement signed by the business associate is not HIPAA compliant, it is counted as a violation as information sharing is not protected by HIPAA laws.
Failure to train staff
Since medical staff are the ones who use and transmit patient information, they have to be properly trained to comply with HIPAA rules. If their training is inadequate, it leaves the door open for more mistakes that lead to HIPAA violation and data breaches.
Failure to protect from device theft
Since devices that hold patient records can be easily stolen, data breaches occur when unprotected or unencrypted devices get lost or stolen. Hence, it is necessary to encrypt all the devices and train staff to prevent theft, in order to avoid HIPAA violation.
Six ways to stay HIPAA compliant
Healthcare providers can be heavily fined for non-compliance. Patient data faces security issues due to IT threats, therefore, being HIPAA compliant is necessary for both patients as well as medical practices. To ensure compliance of HIPAA laws, covered entities and business associates should follow the steps below;
Risk Assessment
HIPAA compliant organizations must identify the risks each year to assess the vulnerabilities in data security. Compliance auditing firms can be hired to assess administrative, technical and physical gaps in safeguarding information. Audits can reveal gaps in compliance of HIPAA rules, which should be followed by remediation of compliance violations. It is important to maintain documentation and fix a timeline for risk assessment and remediation. Organizations can also enlist professional services for their auditing needs. Attorneys and IT auditors specializing in HIPAA compliance can elucidate potential risks and provide guidance to combat breaches.
Security Training
Since sensitive patient information needs to be protected, organizations must train employees to implement HIPAA laws by educating them and minimizing the scope for errors. These trainings help in reducing violations of patient data privacy and shall be conducted at regular intervals. HIPAA training must ensure that the employees understand the regulations and are capable of implementing the protection policies. Such training shows how well-equipped your organization is at preventing data breaches and whether your network is protected.
Documentation
HIPAA compliant organizations should retain all documents pertaining to compliance issues for annual audits. Even HHS and OCR require the availability of proper documentation in the event of a HIPAA investigation. An inventory of all the data regarding PHI and other sensitive records should be managed by the organizations.
Backup of Data
It is crucial to have back-up of patient information files in case there is a breach or loss of data due to unforeseen events. The data back-up should also be stored in external devices such as external hard drives, USB devices, apart from the internal system.
Business Associate Management
It is essential to create policies regarding use and access to PHI. Agreements with business associates should ensure that they will responsibly transmit patient information. The business associates become liable for handling the PHI securely. These agreements should be reviewed at regular intervals to decide accessibility to patient data.
Breach Management
In the event of a data breach, an organization must have a dedicated compliance department to help with the investigation of the breach. The same employees must also be equipped to notify the affected patients and document the proceedings.
The ways listed above will ensure maximum protection of patient data against threats. Ideally, an effective compliance program should include seven fundamental elements advised by the Office of Inspector General (OIG), as quoted below;
- Implementing written policies, procedures and standards of conduct.
- Designating a compliance officer and compliance committee.
- Conducting effective training and education.
- Developing effective lines of communication.
- Conducting internal monitoring and auditing.
- Enforcing standards through well-publicized disciplinary guidelines.
- Responding promptly to detected offenses and undertaking corrective action.

HIPAA compliant software checklist
Apart from the administrative ways discussed above, technical safeguards also ensure that the medical practices using them remain HIPAA compliant. Therefore, healthcare softwares must include certain necessary features. The checklist of these features is given below;
- Data access control and management
The access to e-PHI should only be provided to a few selected employees. To maintain this control, software companies should use unique identifiers for patients and business practice, enforce a multi-tier access policy and automatic logoffs and provide encryption support. Technologies such as biometrics and single sign-on can be used for access management.
- Encryption of data
To ensure the safety of e-PHI, organizations must opt for encryption of patient data using secure website and app development. Only authorized personnel should have access to PHI through passwords or PIN codes. Automatic logoffs are yet another strategy in ensuring prevention of data leak in case the system is left unattended for long.
- Integrity
Preventing unauthorized access is crucial for HIPAA compliance. Use of digital signatures and verification of stored data using PGP, SSL, etc. Multi-factor authentication can also be used for user authorization.
- Data transmission safety
Healthcare softwares should have provision for means of access denial for non-protected communication. The aim is to protect the transmitted data from being intercepted.
What are the benefits of being HIPAA compliant?
Every health provider and associated organizations must be HIPAA compliant not only due to mandates but because of the associated benefits. HIPAA compliant organizations stand to reel in several benefits, which are discussed below;
Trust and loyalty
Covered entities and business associates stand to gain more business if they are HIPAA compliant as patients tend to place their trust in organizations that have been mandated to protect their sensitive health information. HIPAA law compliance ensures confidence in patients that the integrity of PHI is maintained. Since trust breeds loyalty, such patients also become loyal to these organizations and continue their relationship for years and years, which leads to high client retention and better employee morale.
Financial benefits
HIPAA compliant organizations have to make changes in their administration to implement safeguarding of PHI, which results in the smoother and more efficient functioning of the practice. An efficient and compliant organization tends to produce better patient outcomes, which translates into more business and profitability. Patient retention due to loyalty also contributes to better finances.
Standardization
HIPAA rules enforce the standardization of medical records and protect access to them. This increases the efficiency of healthcare professionals to access and transmit health records securely. HIPPA laws ensure that PHI is transmitted under the same code sets along with standard identifiers that aid in transfer of data between different entities.
How to stay HIPAA-compliant while texting
Texting makes communication quicker, easier, and more personal. But in healthcare, it also means being extra careful. Every message can contain sensitive details about someone’s health, and if it falls into the wrong hands, it can be a major issue that ends up in courtrooms instead of inboxes. Respecting the trust and preserving patients’ privacy are the two most important aspects of being HIPAA compliant when texting.
Here’s how to keep your texting practices safe and responsible:
Choose a HIPAA-Compliant Texting Platform
Start with the right tool. Regular messaging apps don’t offer the kind of privacy patients deserve. A HIPAA-compliant platform like Emitrr is made with patient communication in mind, helping you keep every message secure, so you can focus on your conversation without worry.
Enable End-to-End Encryption
Think of encryption as sealing your messages in a locked envelope that only the right person can open. It makes your conversations private, even if someone tries to peek along the way.
Obtain Patient Consent
Before you start texting a patient, make sure they are okay with it. A prompt written note or a HIPAA-compliant online form can do the job for you. It also helps to stick to HIPAA-compliant text message templates so your communication stays clear, consistent, and within the rules. You can download our HIPAA-compliant SMS template PDF here:
Implement Role-Based Access Control
Not everyone needs to see every message. Give texting access only to the team members who genuinely need it. This helps keep things organized and private.
Avoid Using Personal Devices
It might feel convenient to text from your own mobile phone, but it opens too many doors. Stick to work devices or approved systems so messages don’t mix with your personal life.
Set Automatic Logouts
Sometimes we forget to sign out. Automatic logouts provide a contingency plan for your systems to prevent the data from remaining vulnerable if someone leaves their screen open.
Use Two-Factor Authentication
Two-factor authentication adds an extra layer of security before anyone can get in. Even if someone guesses your password, they will still need that second code. This simple step adds a lot of safety.
Maintain Detailed Audit Logs
Maintain a discreet log of who sent what and when while texting communication. These logs are helpful if there is ever a query regarding anything that was shared or disclosed.
Get all the details about HIPAA-compliant texting in this video:
How to maintain HIPAA compliance during VoIP communication
Even a short conversation over a phone call can contain critical information that needs to be protected in the healthcare industry, even though calls may seem safer than texting. Whether it is a voicemail, a follow-up call, or a virtual appointment, every aspect of the exchange counts. The purpose of HIPAA telephone rules for phone conversations is to protect patient privacy; therefore, it is important to get everything set up correctly from the start.
Below are ways to maintain the security and compliance of your VoIP system:
Go for a HIPAA-Compliant VoIP Provider
Patient privacy is not considered meticulously by all VoIP service providers. Choose HIPAA-compliant VoIP software that can provide written documentation to support its HIPAA compliance. These providers offer the right kind of privacy checks from the ground up.
Sign a Business Associate Agreement (BAA)
Before using any VoIP provider, make sure they are prepared to sign a Business Associate Agreement (BAA). This is a simple way of saying, “We’re both in this together, as well as we are both responsible for keeping patient information private.”
Encrypt Call Data and Transmissions
Every call carries data, whether it is live or recorded. Encrypting it means turning that data into code that outsiders cannot read. It is a simple but powerful way to keep conversations safe as they travel across the internet.
Secure Access to Call Logs and Recordings
VoIP systems often store call history and voicemails. That is beneficial, but only if it is protected. Using a HIPAA-compliant voicemail service and speech-to-text tools allows your recordings to be handled with care and stored in safe hands.
Limit Access to Authorized Personnel Only
Access to patient calls is not necessary for every team member. Restricting information to those who “need to know” reduces the possibility of errors or abuse. The fewer the eyes on the data, the safer it stays.
Enable Call Monitoring and Alerts
Set up HIPAA-compliant call tracking and monitoring tools. These help you rectify any unusual activity early on, like access from unknown devices or users, so you can take quick action before it turns into a problem.
Regularly Review Security Settings
Security is not something you set once and forget. Take time every now and then to go over your system settings. Gaps or expired permissions that could otherwise go unnoticed can be found with a quick review.
How to schedule appointments without violating HIPAA guidelines
On the surface, booking an appointment could seem simple: pick a date, set a time, and send a reminder. But when health information is part of the conversation, even small details need to be handled with care. A name, a phone number, and a reason for the visit are all that count. Ensuring that patients can trust how their information is used from the very first interaction is the key focus of HIPAA compliance, and not making things more difficult.
Following are some ways for maintaining a trustworthy, safe, and organized schedule:
Select a HIPAA-Certified Scheduling Tool
Start with a platform built for healthcare. HIPAA-compliant scheduling software will have all the guardrails in place to protect sensitive details and give patients a secure experience from the first click.
Avoid Collecting Excessive PHI
Stick to what is needed to book the visit. If you are using HIPAA-compliant forms via text, keep them short and focused. For example, instead of asking every time, “What symptoms are you experiencing?” you can ask, “Is this appointment for a new or existing concern?” It gets the job done without collecting more than required.
Control Calendar Access with Permissions
Use a HIPAA-compliant calendar that allows you to decide who sees what. Whether it is front desk staff or care teams, everyone should only have access to the parts of the calendar that relate to their job. It is a simple way to prevent accidental oversharing.
Send Appointment Reminders Securely
Use HIPAA-compliant reminder tools, be it for text reminders or emails, to make sure your messages stay private. Appointment reminders should be short and to the point. For example, a text that says, “Reminder: Your appointment at ABC Clinic is scheduled for 3 PM tomorrow” works well. Avoid including names, symptoms, or reasons for the visit. It is one of the best practices for appointment reminders that keeps patient information protected while still being helpful.
With Emitrr’s AI agent, Sarah, your appointment reminders are sent out on time! Here’s how:
Log All Edits and Changes Automatically
People reschedule, cancel, or update their information as plans change. To have a precise record of what was modified and by whom, every such change needs to be automatically logged. If you ever need to go back and comprehend what transpired, this becomes extremely valuable.
Store Data on Encrypted Servers
All appointment data, HIPAA fillable forms, and messages should live on servers that scramble the information so it cannot be read without the right tools. This keeps it safe even if someone tries to snoop.
Review Vendor Compliance and BAA Status
Before using any scheduling tool or platform, double-check that the vendor is HIPAA-compliant and willing to sign a Business Associate Agreement. It is an agreement that shows they are on board with protecting patient information, too.

Frequently Asked Questions
Businesses and entities that adhere to administrative, physical, and technical safeguards mentioned in HIPAA guidelines make them HIPAA compliant.
In order to send HIPAA-compliant messages to patients, you need to use a HIPAA-compliant SMS software like Emitrr.
HIPAA permits medical providers to disclose protected health information (PHI) of an individual to another healthcare provider for case management, coordination of care, treatment, etc.
Conclusion
Healthcare industry relies heavily on HIPAA laws to perform better by implementing safety measures for protection of sensitive patient health information. Covered entities and business associates both follow several rules to become HIPAA compliant in order to safeguard PHI and e-PHI. There are several ways including annual risk assessment, data encryption, documentation, employee training, business associate management, etc, that help organizations to stay HIPAA compliant, while reaping in benefits like patient retention, data standardization and profitability. HIPAA-compliant organizations are most trusted by patients since they ensure that the patient’s privacy is upheld. Both patients and healthcare providers draw immense benefits from HIPAA laws.

 4.9 (400+
reviews)
4.9 (400+
reviews)
