Introduction to Athena Patient Billing
Patient billing is critical to a practice’s cash flow, and Athena patient billing is built to manage claims, payments, and patient balances in one connected system. Still, even small gaps can lead to delayed revenue and patient confusion.
AthenaHealth ties patient billing into its broader revenue cycle workflow, from insurance verification to post-visit payments. In this guide, we explain how Athena patient billing works and where practices may need added support to improve collections and patient experience.
What Is Patient Billing in Healthcare?
Patient billing refers to the process of charging patients for the portion of care not covered by insurance. This includes copays, deductibles, coinsurance, and any self-pay balances. It’s a key part of the broader revenue cycle management (RCM) process.
Patient billing is typically completed following the processing of insurance claims. The patient is responsible for the remaining amount after the payer pays its portion or rejects a portion of the claim. The practice then needs to notify the patient, create a patient statement, and collect payment.
With systems like AthenaHealth, patient billing is closely tied to insurance billing. The accuracy of eligibility checks, coding, and claim submission directly affects how much patients owe and how quickly balances can be collected. Errors earlier in the cycle often show up later as billing disputes or delayed payments.
Understanding patient billing is important not just for practice revenue, but also for patient experience. Clear bills, timely communication, and easy payment options can significantly improve collection rates and reduce frustration.
AthenaHealth’s Patient Billing Workflow: Step by Step
AthenaHealth patient billing is built into its broader medical billing and RCM platform. Instead of handling billing as a separate process, Athena connects patient billing to scheduling, clinical documentation, claims, and payments.
Here’s how the workflow typically works:
- Patient and insurance information is collected during registration.
- Charges are captured after the visit and converted into claims.
- Claims are submitted to payers and processed.
- Payments from insurance are posted.
- Any remaining balance is billed to the patient.
This connected workflow helps reduce manual data entry and billing errors. AthenaHealth uses rules engines and automation to flag potential issues before claims are submitted, which can reduce denials and speed up reimbursement.
However, while AthenaHealth handles the backend billing process well, patient-facing communication and follow-ups often require complementary tools like Emitrr which automates payment reminders, enables two-way patient texting, and helps practices collect balances faster.
Check out this quick video that explains how tools like Emitrr automate patient communication part within Athenahealth:
1. Patient Registration & Insurance Verification
Patient billing begins in AthenaHealth at the front desk. With patient registration, Athena gathers demographic information, insurance information, and eligibility information.
The insurance verification systems offered by AthenaHealth assist medical practices in verifying the
- Active coverage
- Active
- Covered services
- Expected co-pays and deductibles
This step is very important because accurate insurance verification leads to proper billing of patients. A patient’s charges can be estimated properly when eligibility verification is performed at the very start. AthenaHealth enables providers to quickly find self-pay patients and mark accounts that may need up-front payments. This not only enhances patient payment revenue but also prevents bad debt in case of non-payment after a visit.
However, patient billing will not be without hitches if verification is solely used. Patients may end up being puzzled about what they have to pay, especially where deductibles or co-insurance payments are involved. Clear communication at this stage plays a major role in avoiding billing disputes later.

2. Charge Capture & Claim Creation
After the patient visit, AthenaHealth captures charges based on documented services. These charges are then coded using standardized medical coding systems and prepared for claim creation.
AthenaHealth’s billing system includes built-in checks to:
- Validate codes
- Match diagnoses with procedures
- Identify potential claim errors
Once charges are finalized, Athena generates insurance claims electronically. This step is important because inaccurate coding or missing information can lead to denied or delayed claims, ultimately impacting patient billing timelines.
3. Claim Submission & Insurance Processing
AthenaHealth sends claims electronically to insurance companies and tracks them in real time. The system relies on rules and claims processing histories with insurance companies to increase claim acceptance rates.
When a claim is rejected or partially reimbursed, Athena points out these matters for future attention. This is where denial management becomes important. Effective denial handling helps practices recover revenue that might otherwise be passed on to patients incorrectly.
For patient billing, it is very important to have accurate insurance claims processing. Inaccurate claims processing can sometimes cause an increase in patient receivables.
The RCM solutions offered by AthenaHealth can alleviate these challenges, but manual monitoring by staff is necessary, especially in complicated claims and specialty billing.
4. Payment Posting & Reconciliation
Once insurance payments are received, AthenaHealth posts them to patient accounts. The system reconciles:
- Amount billed
- Amount paid by insurance
- Remaining patient responsibility
This step ensures patient balances reflect what is actually owed after insurance adjustments. Accurate payment posting helps prevent overbilling or underbilling patients.
AthenaHealth also tracks contractual adjustments and payer-specific rules, which improves billing accuracy. For practices, this reduces rework and billing corrections later.
At this stage, the patient balance is finalized and ready to be billed.
5. Patient Billing & Statements
After insurance processing, AthenaHealth generates patient statements for any remaining balance. These statements may include charges for copays, deductibles, coinsurance, or self-pay services.
Patients are typically notified through:
- The Athena patient portal
- Email or billing notifications
- Mailed statements (depending on practice setup)
Although AthenaHealth does support patient statements, most practices find this function to be underutilized when it comes to billing communications.
This is where users can add an additional tool like Emitrr into Athena. Emitrr is a complete communication tool that can allow you to automate billing reminders, do HIPAA-compliant two-way texting, set up rules to auto-assign conversations directly to the relevant teams, and so on. The best part is you don’t even have to use two different software, you can enable Emitrr within your Athena dashboard to fill this gap.

6. Digital Patient Payment Options
AthenaHealth enables patients to make payments online via the patient portal. The patients can check their accounts and make payments.
Digital payment options help improve convenience and reduce front-desk workload. Online payments also tend to be faster than traditional check-based collections.
However, patient expectations are evolving. Many patients now prefer:
- Payment links via text or email
- Simple, mobile-friendly payment experiences
- Automated reminders for unpaid bills
Emitrr can again come in handy here and help you fully automate patient payment reminders and follow-ups.
7. Denials & Resolution
Claim denials can greatly affect patient billing statements. When an insurance company fails to reimburse an amount, this results in incorrect patient balances.
AthenaHealth includes denial management tools that help identify:
- Common denial reasons
- Payer-specific issues
- Claims requiring resubmission
A good denial resolution can help in ensuring patients do not end up being charged for more than they need to pay. Otherwise, patient accounts can end up being outstanding because of denied payments. Effective denial management ensures both revenue and patient trust are protected.
Best Practices for Patient Billing With AthenaHealth
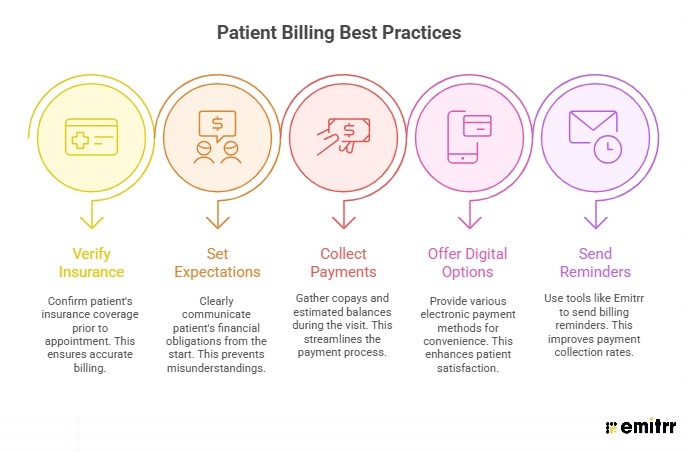
To get the most out of AthenaHealth billing, practices should follow a few best practices:
- Verify insurance eligibility before every visit
- Set clear expectations about patient responsibility upfront
- Collect copays and estimated balances at the point of care
- Offer multiple digital payment options
- Send timely billing reminders and follow-ups by integrating a tool like Emitrr into Athena
While AthenaHealth provides a strong billing foundation, combining it with a communication and automation software can significantly improve patient collections and patient satisfaction.
Common Challenges Practices Face
Even with AthenaHealth, patient billing challenges still exist:
- Patients don’t always understand their bills
- Statements are overlooked or ignored
- Manual follow-ups take time
- Payments are delayed or incomplete
These gaps can lead to growing accounts receivable and frustrated staff. This is why many practices look for ways to enhance patient billing communication beyond the core EHR.
How Emitrr Solves Challenges Within AthenaHealth
AthenaHealth efficiently manages insurance billing, claims, and payment posting. However, many practices find that patient billing challenges begin after the balance is created, that is when patients need to be informed, reminded, and guided to payment.
This is where Emitrr works alongside AthenaHealth to improve patient billing outcomes.
With Emitrr, practices can:
- Automatically send patient reminders to AthenaHealth patients via SMS + Email.
- Share secure text-to-pay links, allowing patients to pay in seconds
- Automate follow-ups for unpaid balances, reducing manual calls
- Text your patients within Athena using Emitrr’s Chrome extension
- Reach patients faster than email or paper statements
By adding automated, mobile-friendly communication to AthenaHealth’s billing workflow, Emitrr helps practices reduce outstanding balances, improve patient response rates, and save staff time, without changing how billing is handled inside Athena.

FAQs: AthenaHealth Patient Billing
Yes, AthenaHealth includes patient billing as part of its revenue cycle management system.
Patients can pay through the Athena patient portal using online payment options.
Basic notifications are supported, but advanced automation often requires additional tools.
AthenaHealth is strong for insurance billing and RCM, but patient payment follow-ups may need enhancement.
AthenaHealth is a cloud-based EHR with built-in billing and revenue cycle tools, while Epic is typically an on-premise or hosted system designed for large health systems. Athena is easier to deploy and manage, whereas Epic offers deeper customization but requires more resources.
AthenaHealth functions as both an EHR and EMR. It stores patient medical records (EMR) and also supports broader data sharing, reporting, and care coordination features commonly associated with an EHR.
How much does Athena cost per month?
AthenaHealth pricing is not fixed. Instead of a flat monthly fee, Athena usually charges a percentage of a practice’s collections, typically ranging from 4% to 7%, depending on services used and practice size.
AthenaHealth is commonly used by small to mid-sized medical practices, outpatient clinics, specialty practices, and some hospitals looking for a cloud-based EHR with integrated billing and RCM tools.
Athena EMR handles billing through an integrated revenue cycle management system. It supports insurance verification, claim creation, claim submission, payment posting, and patient billing after insurance payments are processed.
AthenaHealth is not just billing software. It is an all-in-one platform that includes an EHR, practice management, and medical billing tools, making billing one part of a larger healthcare workflow.
Conclusion
AthenaHealth offers a strong foundation for EHR, insurance billing, and revenue cycle management. It streamlines claims, payments, and patient billing within a single system, making it a reliable choice for many healthcare practices.
However, patient communication and payment follow-ups are two areas where it lacks.This is where layering Emitrr on top of AthenaHealth can make a real difference. Emitrr fills the gaps with automated patient texting, payment reminders, two-way communication, and faster collections, without disrupting your existing Athena workflow.
Together, Athena + Emitrr help practices get paid faster, reduce no-shows, and deliver a better patient experience.
Want to see how Emitrr works alongside AthenaHealth? Book a quick demo and see it in action.

 4.9 (400+
reviews)
4.9 (400+
reviews)