Healthcare was once confined to physical consultation and manual processes. But today, the healthcare industry is evolving into a digital-first industry. With AI’s entry into the picture, everything from diagnosis to patient care is getting a much-needed upgrade.
Among these advancements is a quiet revolution, which is the rise of Virtual Nursing Assistants (VNAs). These intelligent systems are specifically designed to support both healthcare providers and patients. They respond to patient queries, send medication reminders, provide accurate symptom analysis, and free up human nurses for more complex and human-centered tasks. But what exactly are VNAs? How do they work? And what role will they play in the future of healthcare?
In this guide, we will walk you through the journey of VNAs, from their underlying technologies to real-world applications and future trends.
The Evolution of Nursing: From Human-Only to AI-Assisted Care
Before we dive in and understand the specifics, it is important to appreciate how far nursing has come.
Traditionally, nurses have always played a crucial role in patient care. From administering medication, monitoring vitals, documenting patient records, to offering emotional support. But with the modernization of hospitals, the footfall of patients increased, and patient care became more complex; as a consequence of that, nurses became overwhelmed with routine tasks.
And this is where AI steps in.
With innovations like automation, remote monitoring, and concepts like Natural Language Processing (NLP), many time-consuming duties are now being handled by smart systems. This shift does not replace nurses but empowers them.
Let us see how AI has improved nursing support:
- Managing Repetitive Tasks: Automation routine check-ins, reminders, and FAQs.
- Streamlining Communications: Direct interaction between patients and VNAs, reducing the call loads.
- Enhancing Patient Responsiveness: Instant assistance for patients without nurse intervention.
What Is a Virtual Nursing Assistant?
In the current healthcare environment, with nurses stretched thin and patients seeking faster, more convenient care, Virtual Nursing Assistants (VNAs) are filling the gap as trusted, day-and-night assistants. They are not robots from science fiction; they are already employed, behind the scenes, in hospitals, clinics, and even homes.
So, what are they?
A Virtual Nursing Assistant is a computer program, backed by intelligent technologies such as artificial intelligence, that can communicate with patients, interpret their symptoms, remind them to take medication, and even alert actual nurses to possible health issues. It is like having a nurse in your pocket, one who is always available day or night, waiting to assist.
These assistants can do a lot more than just answer basic health questions. They are built to:
- Listen and respond to symptoms. For example, if a patient says, “I’ve been feeling dizzy,” the assistant can ask follow-up questions, log the issue, and offer suggestions or alerts if needed.
- Provide useful advice based on past health history or known circumstances. So if the individual is diabetic or has high blood pressure, the assistant adjusts their answers accordingly.
- Send medication reminders, appointment reminders, or daily health checks, things that are easy to forget but critical to recovery or condition management.
- Loop in healthcare staff when something appears suspicious or lies outside their remit. It is not attempting to supplant nurses; rather, it is a second pair of virtual hands.

What Makes These Assistants Tick? The Technology Behind Them
Behind every effective VNA are a few big-ticket technologies. But you don’t need to have a degree in tech to grasp the fundamentals.
- AI and Machine Learning: These learn with time. The more the patient uses the assistant, the more it can learn patterns and provide appropriate suggestions. For instance, if one describes difficulty sleeping every Tuesday after chemotherapy, the assistant begins to realize that and changes their strategy.
- Natural Language Processing (NLP) and Voice Recognition: These enable the assistant to comprehend the way individuals naturally converse, whether formal symptom report or casually like “I don’t feel too good today.” It can also detect tone and urgency.
- Conversational Interfaces: VNAs are generally simple to use, whether you type on a mobile app or talk to a smart speaker. The idea is to have the interaction feel normal, as if you were talking to an actual person.
How is a Virtual Nursing Assistant Different from a Regular Health App or Chatbot?
That is a fair question. We have all seen those online symptom checkers or hospital apps, and most people think VNAs are just a fancier version of those. But they are quite different and smarter.
For starters, VNAs are not bound to provide canned, one-size-fits-all responses. They have your medical history at their fingertips, can monitor your ongoing care, and can integrate with other systems, such as your EHRs. That means the assistance they provide is much more tailored and more helpful.
In addition, VNAs are:
- More interactive than chatbots, they prompt follow-up questions, answer in context, and escalate as necessary.
- Available across different platforms, whether you are using your phone, a desktop, or even a smart home device.
- Connected to real clinical systems, they are not isolated tools. They are integrated into the workflows of many modern healthcare providers.
Why Do Virtual Nursing Assistants Matter?
They are important because the patients and healthcare providers are both feeling the strain. Nurses are bogged down by redundant tasks such as reminders, check-ins, and non-emergency patient questions. Patients, on the other hand, need quick replies, assistance in the middle of the night, and reassurance when they are not sure if something is important.
For Healthcare Providers:
- VNAs handle the redundant tasks, so nurses can handle the more serious or emotional parts of care.
- They can assist with alleviating burnout, a rising issue in the medical community today.
- Providers are able to allocate their time where it is needed, with patients requiring complicated or hands-on treatment.
For Patients:
- They receive real-time responses, even in the dead of night.
- They are more likely to adhere to their treatment plans, thanks to timely reminders and friendly check-ins.
- And they tend to feel more involved in their care, knowing there is always a line of communication open, even if it’s virtual.
In short, a virtual nursing assistant doesn’t replace human care. But it does provide a layer of smart support that makes the whole system more responsive, efficient, and perhaps most of all human-centered.

Use Cases of Virtual Nursing Assistants
When you hear the term Virtual Nursing Assistant, it might sound futuristic, something that belongs in a sci-fi movie rather than a hospital. But in reality, these digital assistants are already making a big difference in how care is delivered, especially in places where time, resources, and human availability are stretched thin.
Let’s walk through some real-life scenarios where VNAs are not just helpful, they are becoming essential.
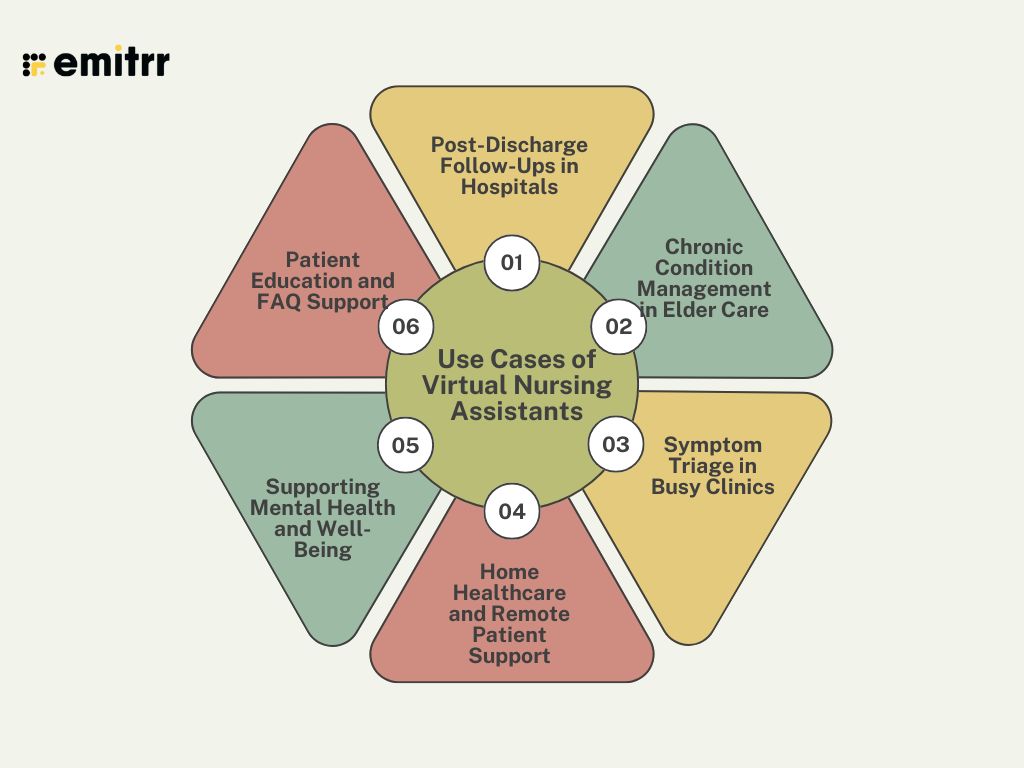
1. Post-Discharge Follow-Ups in Hospitals
One of the trickiest parts of hospital care is not what happens inside the hospital walls, but it is what comes after. Patients often leave with a list of medications, care instructions, and follow-up appointments. But once they get home, confusion or forgetfulness can set in.
That is where a virtual nursing assistant can step in.
Imagine a patient who just had surgery. The VNA checks in daily, asking how they are feeling, whether they are experiencing pain, and if they have taken their meds. If the patient says something concerning, like “I’ve got swelling around the incision,” the VNA can alert a nurse or doctor in real time.
It is like having a digital nurse doing house calls, without the travel.
2. Chronic Condition Management in Elder Care
Older adults, especially those dealing with conditions like diabetes or heart disease, often need consistent monitoring and reminders to stay on track with their care plans. But human caregivers can’t be everywhere at once.
Virtual nursing assistants can help bridge that gap.
Let’s say an 80-year-old living alone has to check her blood pressure twice a day and take five different medications. A VNA can gently remind her, keep a log of her vitals, and even answer basic health questions like, “Is it okay to take this pill with food?”
It adds a layer of support that promotes independence while still keeping safety in check.
3. Symptom Triage in Busy Clinics
In a crowded clinic or urgent care setting, time is everything. Nurses are constantly juggling walk-ins, phone calls, and patient records. That is where VNAs can take on the role of the “first responder”, not in the emergency sense, but in triaging concerns.
For example, when a patient logs into the clinic’s mobile app and types, “I’ve had a sore throat for two days,” the VNA can ask a few follow-up questions: Do you have a fever? Any trouble swallowing? Have you been in contact with anyone sick?
Based on the answers, the system can either offer basic advice or fast-track the patient for a same-day appointment. This kind of digital triage saves time and ensures that urgent issues are not buried under routine ones.
4. Home Healthcare and Remote Patient Support
Many patients today receive care at home, whether due to mobility issues, post-surgery recovery, or a preference for staying out of hospitals. VNAs make home healthcare smarter and more connected.
Take a home health agency that uses a VNA to monitor patients remotely. The assistant might check in every morning with a quick message: “Good morning, how are you feeling today?” Depending on the response, it might offer encouragement, ask more detailed questions, or loop in a nurse if needed.
This type of touchpoint builds trust and ensures that warning signs don’t go unnoticed between in-person visits.
5. Supporting Mental Health and Well-Being
Not all symptoms are physical. Sometimes, a patient just needs someone to talk to.
VNAs are starting to find a role in early mental health support. While they don’t replace therapists or psychiatrists, they can ask basic screening questions, encourage journaling, or remind users to take prescribed medication.
For example, someone managing anxiety might receive a gentle midday nudge: “Take a deep breath. How are you feeling right now?” It’s simple, but it can make a big difference in helping patients feel seen and supported.
6. Patient Education and FAQ Support
Healthcare is full of instructions, terms, and rules that can be confusing, especially for first-time patients. VNAs can help clarify the basics and reduce the need for repetitive nurse explanations.
Think about all the times nurses are asked questions like, “Can I eat before this test?” or “When will my lab results be ready?” A virtual assistant can answer many of these questions instantly and accurately, freeing up the care team to focus on more hands-on needs.
Save time with ready-to-use voicemail greetings for nursing teams. Download and start using them instantly.
The Key Technologies Behind Virtual Nursing Assistants
You don’t need to be a technology guru to find yourself amazed at how virtual nursing assistants (VNAs) work. At the core of these devices are some amazing technologies, but even more, they are made to feel simple and intuitive to the individuals who use them.
Let us take a look at the key technology behind the scenes and how it all comes together to make healthcare smarter, safer, and more responsive.
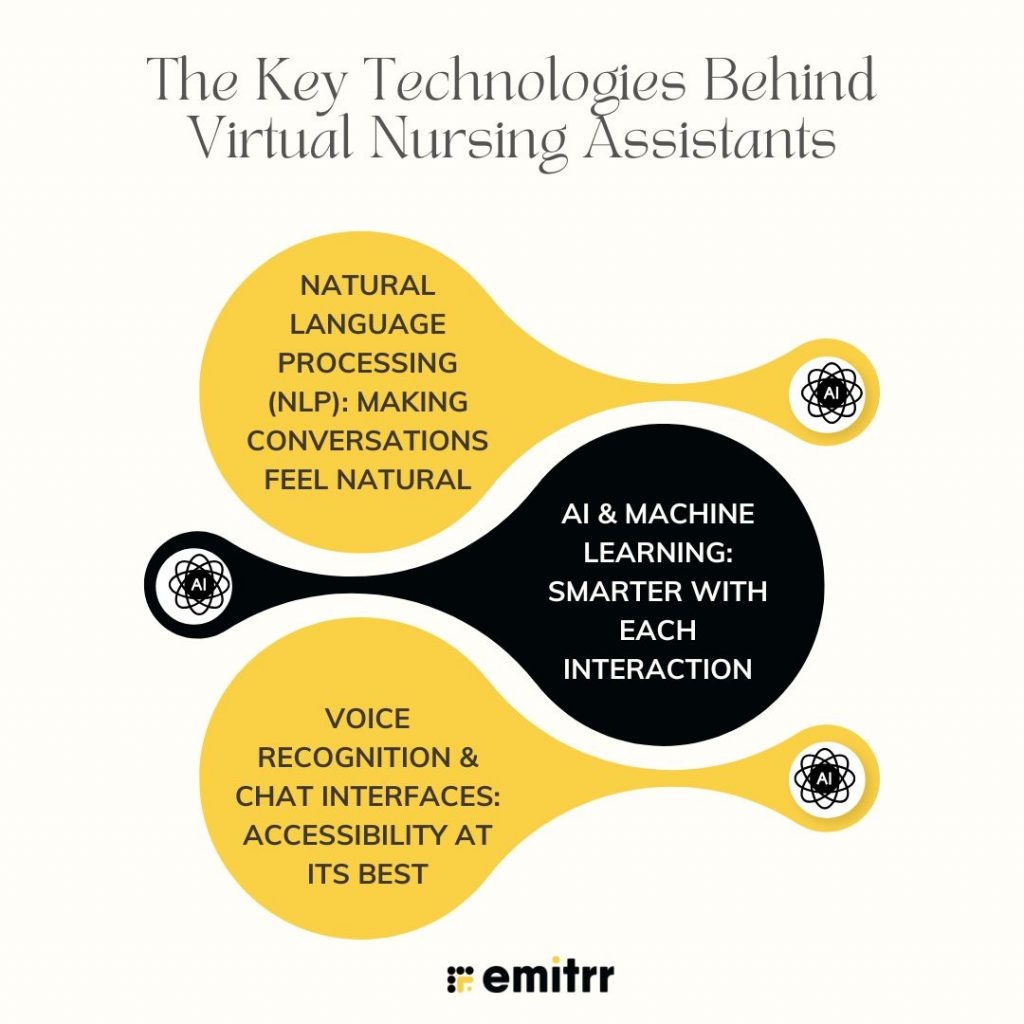
Natural Language Processing (NLP): Making Conversations Feel Natural
One of the first things you will notice about a good VNA is that it understands what you are saying and responds like a human would.
This is where Natural Language Processing, or NLP, is involved. It’s an area of AI that enables machines to comprehend and interpret human language, either typed or spoken.
So when a patient posts something as ambiguous as, “I feel a little dizzy today,” the assistant doesn’t simply read it as words. It is programmed to recognize health-relevant hints. Is dizziness one of the repeated issues? Is it perhaps a medication side effect? Or is something more serious?
NLP enables the assistant to know the context rather than the sentence alone. That is far beyond a standard chatbot.
AI & Machine Learning: Smarter with Each Interaction
AI and machine learning are the VNA’s brain; they make it wiser day after day.
As the assistant deals with dozens, hundreds, or even thousands of patients, they begin to discern patterns. Perhaps it becomes aware that individuals who present with fatigue and shortness of breath tend to end up with a follow-up. Or that specific symptoms recur after a certain treatment.
With time, the VNA gets better at responding. It learns to prioritize what needs urgency, what can wait, and what needs to be escalated to a nurse.
That is why the more it’s used, the better it becomes at being useful and dependable.
Voice Recognition & Chat Interfaces: Accessibility at Its Best
Let’s be real, not everybody will (or can) type out their symptoms on a small phone screen. That is why voice recognition is such a game-changer.
Some virtual nursing assistants simply let patients speak to them no typing involved. It’s particularly useful for seniors, individuals with impaired vision, or those who simply prefer to talk rather than type.
Whether on a mobile app or even a smart speaker, these assistants are positioned to reach patients where they are and communicate how they do. The voice and chat interfaces also make the experience less robotic and more human, which helps in establishing comfort and trust.
Routine Care Made Smart: How VNAs Automate Healthcare Tasks
At their essence, virtual nursing assistants are designed to lighten the load of mundane healthcare for both patients and providers. It’s not merely genius tech; it’s about fixing real, day-to-day issues.
Here’s how they accomplish that.
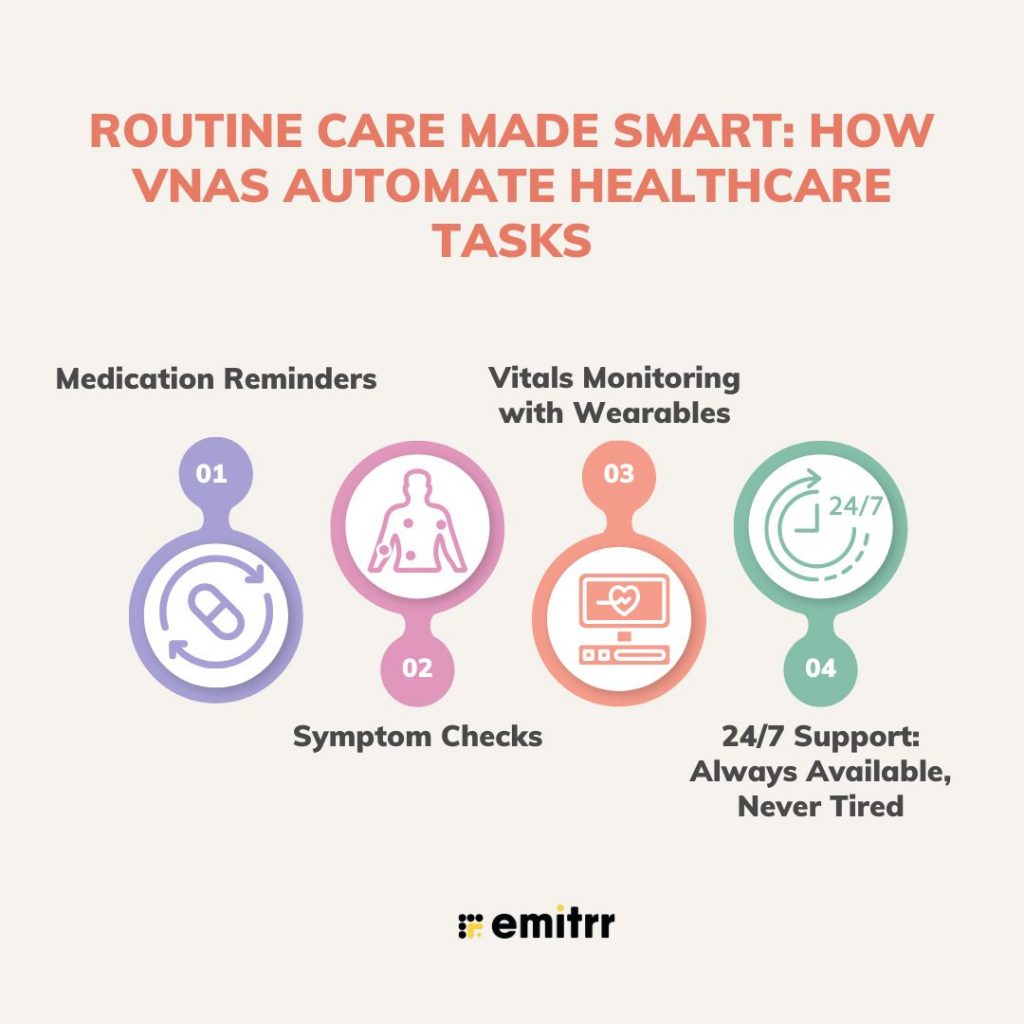
Medication Reminders
We all forget things, particularly when having to manage multiple prescriptions or side effects. VNAs remind patients to stay on schedule with gentle, timely reminders. A simple message reading, “Don’t forget your blood pressure medication at 6 PM,” can make the difference in remaining stable and skipping a dose. This becomes particularly useful for older patients or those who need to manage ongoing conditions.
Symptom Checks
Suppose a patient begins to feel off, perhaps with a cough, some tiredness, or some light chest pain. Rather than waiting for an appointment, they can inform the VNA just what they are feeling. The aide will ask appropriate follow-up questions, determine the severity, and suggest whether it’s something they can do at home or if they need to call a nurse. It’s like triage, except it occurs from your couch.
Vitals Monitoring with Wearables
With fitness bands and smart medical devices, VNAs can be linked to devices that monitor heart rate, oxygen saturation, blood pressure, and so on. If something appears amiss, for instance, an abrupt surge in blood pressure or a jagged heartbeat, the system will notify healthcare professionals instantaneously. It is remote care, but with real-time awareness.
24/7 Support: Always Available, Never Tired
Unlike human personnel who require breaks, VNAs do not punch out. They are present in the dead of night, on the weekends, or on holidays. If someone requires a brief check-in or a reminder, the assistant is there. This constant availability translates to fewer missed issues and quicker intervention when it’s necessary. And for health care professionals, that’s fewer minutes spent on processing routine questions, and more time devoted to up-close, in-person care.
Improving Patient Experience Through Individualization
Let’s be real, healthcare isn’t a one-size-fits-all proposition. People have unique communication, medical, and comfort levels. The best VNAs know that and respond accordingly.
Personalized Communication
A good VNA does not address a 28-year-old post-op patient the same way it addresses an 82-year-old who has memory problems. It may keep things brief and to the point for a patient who wants straight answers, or it may offer more explanation for a patient who asks long questions. It can even change tone and language preference, and even provide translations or regional language options where necessary. That level of customization makes care more human, even when it’s delivered from a screen.
Early Warnings and Predictive Care
VNAs aren’t simply responding; they are anticipating. By looking at trends over time, they are able to identify subtle shifts in a patient’s health that could indicate a problem in the making.
Maybe a patient has been reporting poor sleep, occasional chest pain, and fatigue. Separately, those don’t raise red flags. But together? The assistant might detect a pattern and prompt a follow-up or notify the care team to take a closer look. That kind of proactive care helps catch problems before they become emergencies.
On-Demand Support and Higher Satisfaction
There is something incredibly comforting about knowing you’re not alone in your care journey. VNAs provide immediate access to guidance, clarification of confusing directions, or simply a nag when your day starts to get hectic. That feeling of continuous support of being “checked in on” typically translates to increased trust and satisfaction with the overall care experience. It’s not about responding to questions; it’s about establishing a patient-care system relationship even when it’s electronic.

Real-World Applications: Case Studies of Virtual Nursing Assistants
Virtual Nursing Assistants (VNAs) are not just tech showpieces; they are already being used in the real world to solve real problems. From busy hospitals to rural care setups, these digital helpers are quietly but significantly transforming how healthcare gets delivered.
Let us take a look at how VNAs are making a difference in different healthcare environments:
1. Hospital Systems: Easing the Post-Discharge Burden
One major hospital chain in the U.S. decided to try out VNAs to help with a common pain point: managing patients after they have been discharged.
Normally, this involves a lot of follow-up calls from nurses, checking if patients are taking their meds, monitoring for complications, and making sure appointments are scheduled. It’s essential, but it’s also time-consuming.
By bringing in VNAs to handle the routine parts of follow-up, like sending medication reminders, asking simple symptom-check questions, and flagging warning signs, the hospital saw some impressive results:
- Nurses reported a 30% drop in workload, especially around admin-heavy follow-ups.
- Readmission rates went down by 12%, likely because patients were staying more engaged with their care after going home.
- And perhaps most meaningfully, nurses said they felt less overwhelmed, with more time to focus on patients who needed their full attention.
This is a great example of VNAs supporting, not replacing, human care. The tech handled the repetitive stuff, and the nurses could do what they do best.
2. Elder Care Facility: Supporting Seniors with Everyday Needs
At a senior living community, the care team introduced a virtual nursing assistant to help manage ongoing health needs. These were not acute patients; they were mostly seniors living with long-term conditions like arthritis, diabetes, or heart issues.
The assistant was set up to check in daily, asking how residents felt, whether they’d taken their meds, and if they had any new symptoms to report.
Over time, something interesting happened:
- Chronic condition management improved. Residents were more consistent with their routines, thanks to the daily reminders.
- The regular interactions had a positive effect on mental health. Some residents said they felt less lonely knowing someone, even a digital someone, was checking in.
- Families noticed, too. The assistant sent regular health summaries to caregivers and relatives, giving them peace of mind.
In a setting where human staff can’t be everywhere all the time, the VNA became a gentle, supportive presence always available, always listening.
3. Home Healthcare Startup: Bridging the Rural Healthcare Gap
A growing home healthcare startup faced a challenge: how to deliver consistent care to patients scattered across rural regions, where in-person visits weren’t always possible or practical.
Their solution is a virtual nursing assistant embedded into their mobile care platform.
- The assistant helped patients track symptoms, manage their meds, and report vitals, all through their phones.
- It offered multilingual support, which was essential for the diverse communities they served.
- And perhaps most importantly, it reduced the need for constant travel, freeing up nurses to focus their in-person visits on patients with urgent needs.
By combining smart tech with a personal touch, the startup made care more efficient, scalable, and inclusive even across vast, underserved areas.
Help nurses manage patient calls with clear, friendly voicemail greetings. Download professionally written scripts today.
Integration with Healthcare Infrastructure
Now, the thing is rolling out a virtual nursing assistant isn’t like installing a new app and calling it a day. For VNAs to really work, they need to be thoughtfully woven into your existing healthcare systems.
Here’s what that looks like in practice:
1. Assess System Compatibility
Before bringing in any new tech, healthcare providers need to take a close look at what they already use. That means checking whether the VNA can sync with EHR systems, patient communication tools, wearable integrations, and compliance platforms. If the systems don’t talk to each other, you’ll end up with more problems than you solve.
2. Choose the Right Platform
Not all VNAs are created equal. Some are better for hospital discharge workflows, others for long-term care, and others still for remote monitoring. The key is to match the platform to your care goals. Want fewer readmissions? Focus on a VNA with smart follow-up and predictive tracking features. Need support for an elderly population? Look for voice interfaces and medication management tools.
3. Train Your Staff and Set Clear Expectations
One of the most important and often overlooked steps is making sure your nurses, doctors, and care coordinators know how the VNA fits into their workflow. When the team is properly trained and sees the VNA as a tool (not a threat), adoption becomes much smoother. It becomes part of how care gets done, not a clunky layer that slows things down.
Privacy, Ethics, and Compliance in AI-Enabled Care
VNAs handle some of the most sensitive data in a person’s life, their health records. That’s why security and trust are non-negotiable.
HIPAA Compliance Is a Must
Any VNA used in the U.S. (and similar regulations apply globally) must meet strict healthcare privacy standards. This includes how data is collected, stored, accessed, and shared. Providers must be able to prove that the system is HIPAA-compliant, with audits and protections in place.
Encryption and Secure Access
All conversations, health logs, and symptom reports should be end-to-end encrypted. That means even if someone intercepted the data (which is rare), it would be unreadable without the proper credentials. Only authorized users, like nurses or a designated caregiver, should be able to access patient records or live conversations.
Designing with Ethics and Transparency
Patients should know when they are speaking to a digital assistant, and they should feel confident that it’s offering evidence-based responses, not just scripted suggestions.
Trust is built when people understand how a tool works, what it knows, and where the limits are. Ethical VNAs are upfront, transparent, and designed with human dignity in mind.
Voice AI in Virtual Nursing Assistants: A Game-Changer for Accessibility
One of the most promising developments in VNA technology is Voice-based support. Especially for older adults, people with disabilities, or those who aren’t comfortable typing, this can make a huge difference.
1. Voice-Based Interfaces for Seniors
Let’s face it, navigating a touchscreen or a tiny app can be frustrating. But talking? That feels natural.
VNAs that support voice interaction allow seniors to simply speak their symptoms, ask questions, or get reminders, just like they would with a caregiver. No scrolling, no typing, no tech intimidation.
2. Real-Time Transcription and Clinical Triage
For nurses, voice data can be transcribed and reviewed in real time. If a patient says, “My chest feels tight today,” the system logs it and can flag it for clinical review. This helps prioritize follow-ups and avoid missed red flags.
3. Recognizing Emotion Through Tone
Some VNAs are even trained to detect emotional cues in speech, things like hesitation, stress, or sadness.
This is not about diagnosing mood disorders, but it can help flag situations where a check-in might need to go beyond the clinical. If someone sounds distressed, the system can notify a nurse to intervene sooner.
Future Trends in Virtual Nursing Assistants
Healthcare tech’s future isn’t about replacing humans; it’s about making care more intelligent, more personal, and more accessible. Virtual nursing assistants are right at the center of that change, transforming in ways that feel less robotic and more like genuine care partners.
Here is a look at where things are going:
AI + Wearables: Real-Time, Personalized Care at Your Fingertips
We already see VNAs co-existing with fitness trackers and smartwatches. Next, though? Unobtrusive, real-time syncing with medical-grade equipment, such as continuous glucose monitors or smart blood pressure cuffs. Think about it: you take your vitals one morning, and the assistant doesn’t just log it, but says, “Appears your blood sugar’s a tad higher today. Did you forget your evening dose yesterday?” It’s a reassuring reminder, like a nurse catching something tiny before it turns into something big. This type of real-time information aids in making care proactive instead of reactive. It’s not tracking; it’s acting in the moment.
Emotional AI: A Listening Ear, Not Just a Voice Command
VNAs are beginning to do more than simply record symptoms or book appointments. It is being trained by developers to notice how individuals sound, if their voice shakes, slows, or is abnormally silent.
Why is this important? Because emotional changes tend to appear before someone is willing or able to discuss what’s happening. If the assistant notices a pattern of expressions that indicate anxiety, tiredness, or mild depression, it can reply softly, perhaps with a comment such as, “You seem a little down, would you like to speak to someone today? It’s a brief moment, but to one who is quietly struggling, it could be the lifeline they didn’t even realize they needed.
Decentralized Healthcare: Reaching the Unreached
Care access remains a gigantic challenge, particularly out in the rural areas where clinics are miles apart, and doctors are scarce. VNAs are bridging that gap by providing residents of those communities with a consistent means of asking questions, monitoring symptoms, and staying on their game. Imagine a rural mom confirming her baby’s fever using a voice assistant, or an older patient receiving daily reminders in their language. Small shifts like these can add up, and they’re occurring without having to use Wi-Fi or fancy apps. By eliminating geographic and linguistic barriers, VNAs are bringing care to the doorsteps of individuals who’ve so often been left behind.
Emitrr as a Leading Virtual Nursing Assistant Platform
When it comes to virtual nursing assistants, there is one name that keeps popping up in healthcare conversations, which is Emitrr. Whether you are in a hospital setting, a home healthcare service, or a senior care facility, Emitrr is earning a reputation for doing what many platforms promise but few deliver intelligent, reliable, and truly helpful patient support.
So what makes Emitrr stand out in a crowded field of digital health tools?
Why Emitrr Is Turning Heads
1. AI-Powered Automation That Works: Automation can sometimes feel clunky or impersonal. But Emitrr gets it right. Its AI is built to do more than just spit out generic responses. It triages patient needs, handles frequently asked questions, and knows when to hand things off to a real nurse if the situation gets complex.
So when a patient says, “I’ve been having chest tightness on and off,” Emitrr doesn’t just reply with a canned message. It digs deeper, asks the right follow-up questions, and ensures the issue is escalated if needed. It’s like having a frontline nurse assistant who never misses a beat.
2. Easy Integration into Existing Systems: One of the biggest hurdles in adopting new healthcare tech? Integration. If a tool doesn’t play nice with your existing EHR or care coordination platform, it becomes more of a headache than a help. Emitrr was built with that in mind. It connects smoothly with major electronic health record systems, so your team doesn’t need to jump through hoops or redo workflows. Whether you’re using Athenahealth, Epic, or another platform, onboarding Emitrr is remarkably painless, which is music to any IT manager’s ears.
3. Real-Time Communication That Patients Use: We have all seen platforms that claim to “engage patients”, only to require logins, passwords, and clunky portals. Emitrr keeps it simple. It offers real-time communication through SMS, voice calls, and chat, so patients can interact in the way that feels most natural to them. Whether someone is confirming an appointment via text, checking symptoms over the phone, or chatting about medication side effects, Emitrr is right there. The best part? Patients don’t need to download an app or remember another login, making adoption much easier, especially for elderly users.

Key Features That Make a Real Difference
Emitrr doesn’t just talk a good game, its features are rooted in solving day-to-day problems that care teams and patients face.
- Conversational Symptom Checking: Patients can describe how they are feeling in plain language, like “My legs feel swollen again,” and Emitrr responds with questions or advice tailored to their condition. It feels like a conversation, not a questionnaire.
- Multilingual Support: In today’s diverse patient population, language can be a barrier to care. Emitrr supports multiple languages, making it accessible for patients who may feel more comfortable speaking in their native tongue. That builds trust and better compliance.
- Custom Alerts for Vitals, Medications, and Appointments: Emitrr can be programmed to remind patients when it’s time to take medication, track vital signs, or head in for their next checkup. Care teams can even set thresholds, so they get alerts when something looks off, like a missed dose or a high blood pressure reading.
Success Stories That Prove Its Impact
What sets Emitrr apart is the way it delivers measurable results, not in theory, but in the real world.
- A mid-sized clinic reported a 40% drop in no-show appointments after integrating Emitrr’s smart reminders and follow-up features. Patients appreciated the helpful nudges, and the staff spent less time chasing down confirmations.
- A senior care home using Emitrr saw a 25% improvement in medication adherence. Residents received clear, timely reminders, and staff could check in only when needed, rather than constantly hovering. The result? Fewer missed doses and a greater sense of independence among residents.
- Home health agencies using Emitrr noted a significant boost in patient engagement, especially in remote areas. Patients were responding more quickly to check-ins, logging symptoms regularly, and reaching out when something didn’t feel right. That kind of proactive behavior leads to better outcomes and happier patients.
FAQs
VNAs interact with patients through voice or chat interfaces, triage symptoms, send reminders, and alert nurses when necessary, all in real time.
Yes, credible VNA platforms like Emitrr follow HIPAA guidelines and use secure encryption methods for data handling.
No. VNAs are support tools. They enhance, not replace, human care by automating routine tasks and allowing nurses to focus on complex care.
Many VNAs are voice-based, making them easier for seniors to use. Some platforms also support regional languages and simplified commands.
Costs vary based on the scale and features. However, most platforms offer flexible pricing, and the ROI in terms of efficiency and satisfaction is typically high.
Conclusion
Virtual Nursing Assistants are not substituting for nurses; they are complementing them. By taking over onerous tasks, improving patient interaction, and enabling remote care, VNAs are transforming the delivery of healthcare in the quietest, most insidious way possible. Whether you’re a hospital administrator, a nurse, or a technology aficionado, embracing VNAs is about embracing the future of caring, accessible, and savvy care. The sooner you adopt, the greater value you reap for your staff and patients.

 4.9 (400+
reviews)
4.9 (400+
reviews)
