Introduction
Oncology is a complex and demanding field of medicine that focuses on preventing, diagnosing, and treating cancer.. The risks are at their maximum: cancer is the second major cause of death all over the world, and its various forms require highly individualised and prompt interventions in most cases. While cancer incidence remains on an upward trend, the demand for accuracy, rapidity, and reliability in the delivery of services similarly grows. AI steps in here and thus is beginning to assume a very important role.
AI in oncology has moved to the present from the distant future—it’s no longer a dream but a gradually unfolding scenario. For instance, uncovering minute patterns in diagnostic scans, using AI technologies to help clinicians detect cancer earlier, and planning treatments more efficiently are some of the ways in which AI supports healthcare professionals. Businesses enabled by machine learning, deep learning, and natural language processing are now progressively woven into nearly every stage of the cancer journey.
With a system like LYNA (Lymph Node Assistant) developed by Google, AI has been shown to virtually reach perfection in the task of identifying breast cancer metastases. Similarly, the IBM Watson for Oncology tool assists oncologists by analysing extensive medical research and computing patient data to provide evidence-based treatment recommendations. Besides that, these technologies continue to allow increased diagnostic accuracy, and they also reduce the burden of clinician workload as well as facilitate personalised care paths.
With ongoing AI advancements, the technology is not aiming to replace oncologists but is complementing them by facilitating faster, more intelligent, and widely accessible cancer care. This article outlines numerous applications of AI technology in oncology, the positive effects and possible problems caused by the technology, as well as the future of one of the most vital missions of medicine.
Use Cases: Where AI is Being Used in Oncology Today
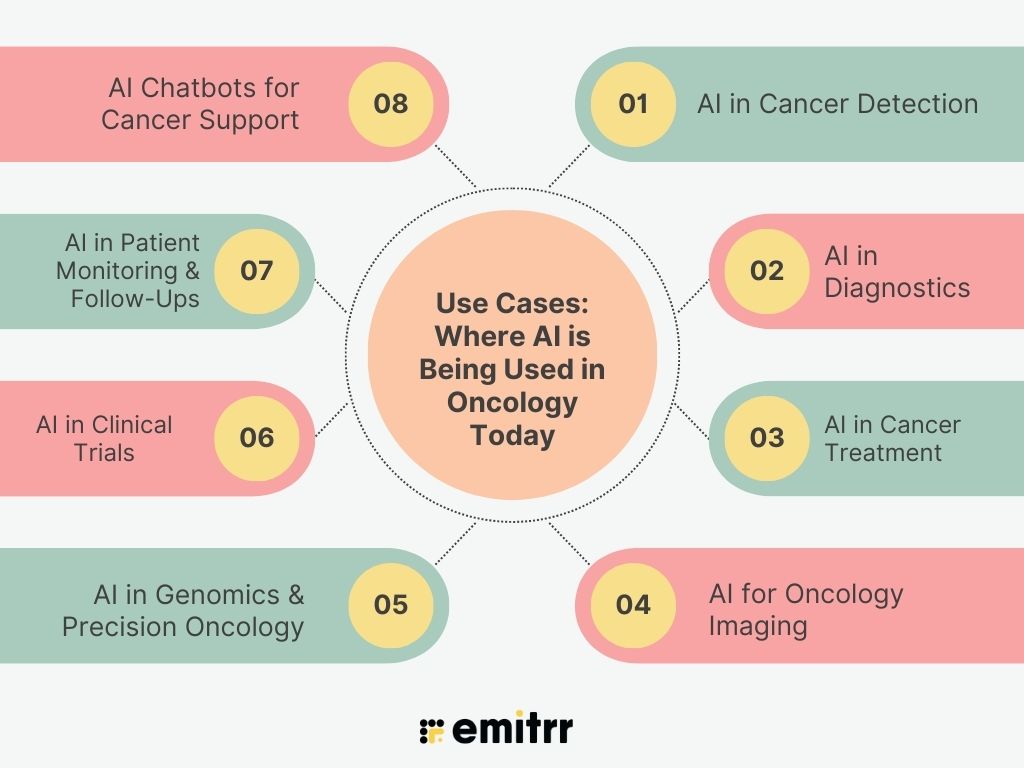
1. AI in Cancer Detection
AI models have shown that they can identify cancer at the initial stages in various types of cancer, e.g., the breast, skin, lung, and colorectal ones. A few leading examples are listed here:
- Skin and breast cancers: Deep learning algorithms that have been trained on tens of thousands of images can differentiate between malignant melanoma and benign lesions with accuracy similar to, or even higher than, expert dermatologists and radiologists
- Lung and colorectal cancer: High-end image-processing networks (such as capsule networks, CNNs) have reached more than 95% accuracy in detecting cancerous tissue from CT and histopathology scans.
2. AI in Diagnostics
AI is not only useful in detection, but it also assists in tumour grading and metastasis prediction:
- Tumour staging and grading: Convolutional neural networks (CNNs) and deep learning models study pathology slides to tell apart benign from aggressive tumours exactly, thus, for example, clinicians can prioritise the cases.
- Metastasis forecasting: Big text and picture models can spy out the tiny metastases in the lymph nodes to decide the treatment course more accurately.
3. AI in Cancer Treatment
AI improves the scheduling and personalisation of treatment therapies:
- Radiation therapy: Systems that are AI-powered decide the best dosage, beam angles, and target volumes, and thus they contribute to the minimum radiation reaching healthy tissues.
- Precision medicine: AI mines through genomics, transcriptomics, and clinical data to suggest treatment plans that fit the patient and find biomarkers that correspond to the treatment.
4. AI for Oncology Imaging
In imaging diagnostics, AI enables:
- Enhanced image processing: Algorithms help MRI, CT, and digital pathology images become sharper and annotated automatically, thus reducing the diagnostic latency.
- Real-time decision support: AR-driven microscopes provide AI-based signal overlays on pathology slides, hence allowing for a faster identification of cancerous cells.
5. AI in Genomics & Precision Oncology
AI has a fundamental impact on the research of genomic and multi-omics datasets:
- Mutation detection: AI methods read gene expression and sequence data to locate driver mutations and predict tumour biology that leads to the design of personalised targeted therapies such as HER2 blockers or immunotherapy.
- Biomarker discovery: Initially, the introduction of basic ML algorithms to research those vast clinical, molecular, and pathological datasets resulted in quite a number of new predictive biomarkers.
6. AI in Clinical Trials
AI makes clinical trial design and patient enrollment more efficient:
- Patient-trial matching: NLP and structured-data analysis platforms rapidly screen medical records and genetics to match patients to suitable trials, boosting enrollment by 3 – 4× times.
- Outcome prediction and adaptive trials: AI models anticipate how patients may respond to therapies, optimising trial design and improving statistical power.
7. AI in Patient Monitoring & Follow-Ups
AI-powered instruments are highly helpful in continuously relieving the burden of patients from one place to another outside the clinic:
- Wearables & symptom tracking: An AI-powered system is no different from a physician’s role— it just keeps the patient monitored 24/7 and raises the alarm when it observes something unusual, such as signs of cardiac toxicity.
- Remote check-ins: Chatbots collect patient-reported symptoms and alert doctors to relevant changes, improving patient engagement and timely care.
8. AI Chatbots for Cancer Support
NLP-powered chat assistants are revolutionising patient interaction:
- Cancer helplines: The use of AI chatbots can free up human resources from repetitive tasks such as answering FAQs, sending appointment reminders, and offering informational support.
- Patient education: Such instruments transform the complicated medical information into more easily understood formats that take into account the individual patient’s needs.
AI in the field of cancer is going through a rapid transformation, ranging from the very early detection and diagnostics to treatment planning, monitoring, and even trial optimisation. The introduction of these new technologies leads to higher accuracy of diagnosis and more effective treatment, besides the improved patient experience and more efficient operations. Responsible introduction of real-life applications is thus necessary to guarantee that care is distributed fairly, safety is ensured, and the features are understandable in cancer treatment.

Benefits of AI in Oncology
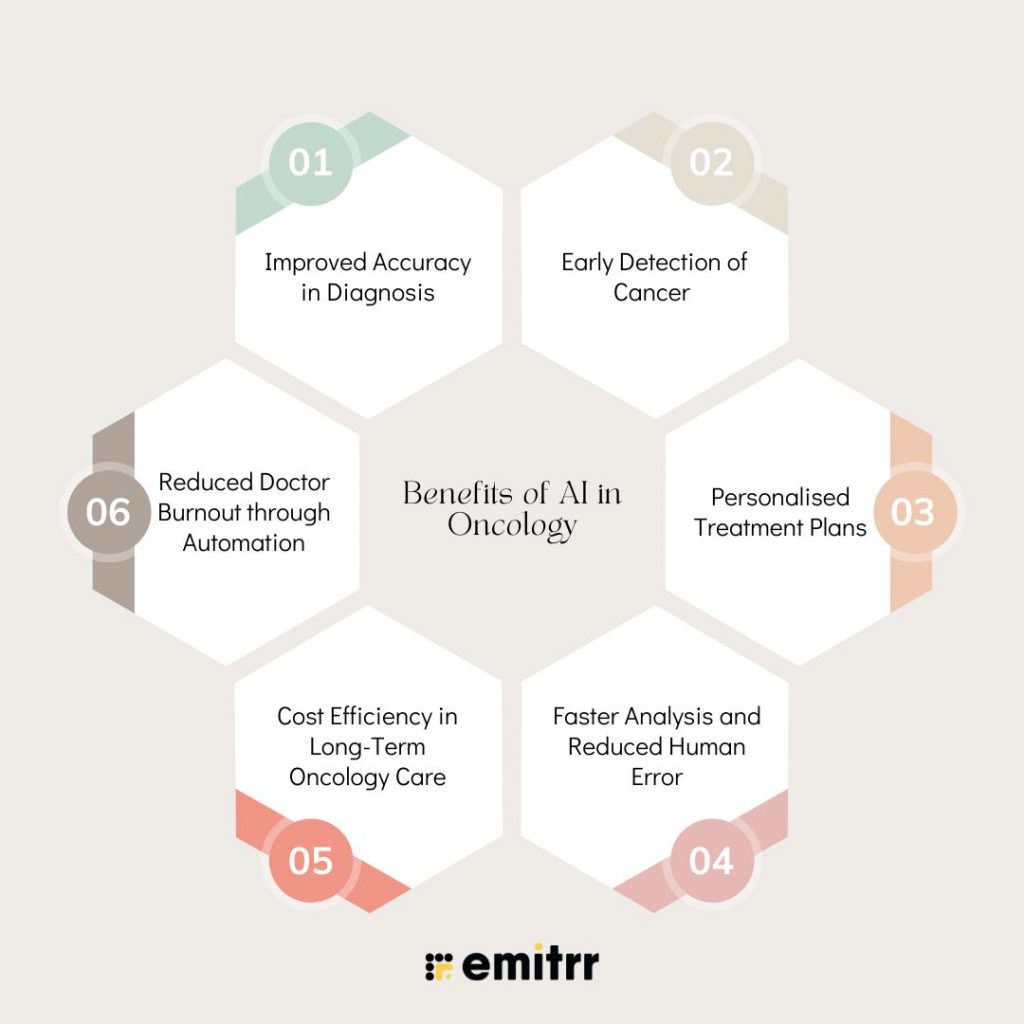
1. Improved Accuracy in Diagnosis
Artificial Intelligence algorithms are designed to comprehend medical data that is complicated by nature, such as radiology scans, pathology slides and histopathological images, thereby helping with diagnosis that is often more accurate than a human one. For instance, machine-learning ventures in oncology have now become so routine that they surpass physicians in deciding between benign and malignant tumours. In research, AI systems showed better results in breast and lung cancer detection and staging than clinicians.
2. Early Detection of Cancer
Most essentially, through the detection of slight patterns in images and biomarkers, AI allows for earlier detection of cancer, which is indispensable to a patient’s good prognosis. It has been proven by the latest study done at UCLA that the AI-enabled analytics tool that is FDA-approved can identify prostate cancer with 84% accuracy, which is far more than the 67% accuracy that doctors achieved. The latter allowed for precise targeting of treatments with reduced undesired effects.
3. Personalised Treatment Plans
AI combines genomics, imaging, and the patient’s clinical history to build specially targeted therapies. Machine learning technologies are always better than conventional methods for statistics in predicting how a patient will respond to the treatment, thus guiding oncologists in formulating the most appropriate treatment plan. These algorithms can be adjusted constantly with new patient information, so precision medicine is no longer limited and can reach more places.
4. Faster Analysis and Reduced Human Error
The decision support tools assisted by AI can interpret the diagnostic data quickly, highlight unusual features, compose radiology reports, or focus on the cases with the most serious findings. Researches illustrate that the change of radiology workflows that are through AI is possible to reduce the reporting time drastically, with no accuracy loss, and thus make the diagnosis and treatment start faster.
5. Cost Efficiency in Long-Term Oncology Care
The use of AI eliminates not only diagnostic, but also treatment-associated costs by streamlining the workflow and increasing the capacity. A simulation demonstrates that the employment of AI-driven treatment solutions in hospitals can result in savings of over USD 289,000 a day by the tenth year, mainly because of time savings and the reallocation of resources.
6. Reduced Doctor Burnout through Automation
AI is capable of relieving clinicians of administrative burdens triage conversations, patient reminders, and EHR updates. Work after-hours is significantly reduced by the use of ambient voice AI scribes and intelligent response systems, which also reduce daily clinician stress. Oncology programs display a measurable reduction in clinician burnout and more focus on patient care.
AI empowers oncologists to deliver more accurate, efficient, and personalised care. Its benefits, ranging from better diagnostics and treatment planning to lower costs and improved clinician well-being, are rapidly being validated in real-world settings. As AI adoption grows, healthcare systems must continue prioritising transparency, equity, and clinician engagement to fully realise the potential of AI in the fight against cancer.
Challenges & Limitations of AI in Oncology
1. Data Quality & Availability
Artificial Intelligence (AI) requires enormous, varied and highly annotated data for training. On the other hand, the inconsistency in the oncological data may adversely affect this as image formats, staining protocols, and document styles differ from one center to another. When datasets are too small or too homogeneous, they negatively affect the model’s ability to perform and be generalizable, while the continuous changes in practice over time may result in performance drift phenomena.
2. Bias in AI Models
Such bias occurs if the training data under-represents certain populations, e.g., ethnic minorities or rare cancers. This would imply that these groups are not served with the same level of accuracy or, worse, that they receive a misdiagnosis. For instance, an algorithm trained on samples that mostly belong to the White race may be unable to find cancer in Black patients—it is just one of many issues that must be dealt with by gathering data from more diverse populations and bias-aware methodologies.
3. Lack of Standardisation Across Hospitals
The changes in technology and the working methods that include the use of different imaging machines, different staining processes, different EHR systems, etc., restrict the AI tools from becoming scalable. Unless standardisation of data collection and processing protocols is implemented, AI models may end up failing if they are applied beyond their original development site.
4. Regulatory & Ethical Barriers
While regulations for AI tools in oncology (such as those from the FDA, GDPR, or HIPAA) are in place, these are frequently lacking and/or outdated compared to the rapid development in the AI field. The same applies to issues related to transparency, accountability, patient consent, and data security.
5. Trust Deficit Among Oncologists & Patients
AI systems are usually “black boxes” that don’t provide any explainability. When doctors can’t figure out how a decision has been made, they are not likely to trust it. Issues related to errors made by AI and accountability could lead to patients and physicians being reluctant to use these devices.
6. Cost of Implementation in Small Clinics
The high expenses for IT infrastructure, model development, validation, and continuous maintenance make it almost impossible for smaller or rural clinics to adopt AI. If there are no cost-effective solutions for AI, it might make healthcare disparities even worse.
AI can revolutionise the field of oncology; however, there are still a number of major issues that need to be resolved. Some of these issues are about making sure the data is diverse and of good quality, bias reduction, clinical practice standardisation, complying with regulations, gaining trust, and finding ways to overcome cost barriers.

How Does AI-Based Communication in Oncology Differ from Traditional Communication?
Effective communication is very important in oncology, where patients deal with difficult treatments and have psychological problems. Traditional human-led processes heavily rely on the systems that are, however, AI is changing communication into faster, smarter, and more personalised. Here is a clear picture of the differences between AI and traditional communication in cancer care:
1. Speed and Availability
Traditional Approach:
Communication is mostly restricted to clinic hours and depends on the availability of the staff. Patients may have to wait for hours or even days for a response, especially out of working hours or on weekends.
AI Approach:
AI-powered chatbots and virtual assistants are there all the time. Patients can schedule visits, get news, and clear their doubts immediately; thus, the care goes on uninterrupted even beyond regular hours.
2. Personalisation and Context-Awareness
Traditional Approach:
Patients generally get standard instructions, leaflets, or answers over the phone from the staff according to a script, with no personalisation related to their disease or treatment stage.
AI Approach:
AI generates messages tailored to each patient based on information such as diagnosis, treatment, symptoms, and even personality. For example, a patient who is on chemotherapy might get personalised diet instructions or meds for nausea as a reminder.
3. Proactive Engagement
Traditional Approach:
Most of the conversation is reactive; patients have to contact the doctor to share their symptoms or ask for information. Follow-ups are often manual and inconsistent.
AI Approach:
AI supports initiative engagement. Machines become the main force in continual actions; they send messages to keep in contact, get the patient’s consent, and detect the early stages of the disease. This is an important efficiency of adherence; it also enables the early detection of complications.
4. Multilingual and Inclusive Communication
Traditional Approach:
There is a very limited number of languages that can be offered by the staff. If a patient comes from a different language background, he can still be a problem to the people who are taking care of him because he won’t understand their language perfectly.
AI Approach:
The AI has the possibility to use more than one language, it can interpret the speech immediately, and it can even provide formats that are the most accessible for the users (e.g., voice or simplified text), ensuring that no patient is left behind due to language or literacy gaps.
5. Data-Driven and Integrated
Traditional Approach:
Communication is mostly when it is outside the patient’s official record — phone calls, notes, or informal updates may not be documented, or if they are, they may not be centralised.
AI Approach:
Additionally, AI systems record conversations with chatbots and symptom reports along with all other interactions and insert them into EHRs. This allows doctors to have a better understanding of the patient’s situation through the provision of up-to-date context.
6. Emotional Intelligence and Human Touch
Traditional Approach:
In particular, face-to-face interaction provides emotional support and the opportunity to discuss sensitive issues, such as life-threatening diseases like cancer, which is of great importance.
AI Approach:
AI technology is not able to create real empathy with humans, but at the same time, it has the potential to significantly reduce the administrative burden of clinicians. As a result, more time will be available for healthcare professionals to have emotionally sensitive conversations with their patients.
Real-World Application:
Emitrr’s AI communication platform takes care of those routines, such as symptom triage, appointment scheduling, and patient FAQs that would otherwise take up most of the time of the cancer clinics. Thus, oncology clinics can keep real-time communication without exhausting clinical staff.
The many good points of AI in oncology communication, like speed, personalisation, and scalability, basically make it very suitable for solving a large part of the problems of traditional systems. Even though AI cannot replace human interaction, it is still very useful in improving patient care since it guarantees that every message is received, every follow-up is recorded, and every patient gets help.
| Aspect | Traditional | AI-Based |
| Availability | Limited hours, staff-dependent | 24/7 support via bots & automation |
| Personalization | Generic, one-size-fits-all | Tailored to patient data & context |
| Engagement | Reactive, patient-initiated | Proactive check-ins & alerts |
| Language Access | Language-limited | Multilingual & inclusive |
| Data Integration | Often siloed or manual | Synced with EHRs and digital tools |
| Empathy | High — human-driven | Supports doctors, lacks emotional nuance |
Where AI Overtakes Human Capabilities in Oncology
AI is superior to humans in tasks where rapid data processing, pattern recognition, and knowledge retrieval at scale are necessary. The main areas are:
1. Image-Based Cancer Detection
Decision-making algorithms that implement the example of Google’s LINA or IBM’s dermatology teams can unravel the most hidden features of images of mammograms, skin lesions, and CT scans, while the accuracy of generalist radiologists is adjusted downwards.
2. Genomic Data Analysis
AI can ingest, analyse, and organise an exponential amount of genetic data in a very short time for the rapid identification of mutations and biomarkers that will guide treatment. It is a feat that no human can accomplish in that time.
3. Clinical Decision Support
Tools such as Watson for Oncology run through an unthinkable number of sources of various sorts, case studies, guidelines, research papers, work in the field, and select those most relevant for the current situation, a process requiring months of human work now being done in seconds.
Where Human Intelligence Still Leads in Oncology
While AI is good at some things, oncologists could hardly be seen as replaceable in areas of this scope that require the understanding of context, compassion, and good judgment.
1. Empathy and Patient Communication
A very human need, such as getting a cancer diagnosis or emotional support throughout the treatment, can be fulfilled by human warmth, cultural sensitivity, and empathy only, areas where AI is still unable to keep up with a human.
2. Handling Complex or Rare Cases
In uncommon or borderline situations, oncologists exhibit subtle reasoning that substantially surpasses data – they essentially combine their understanding, intuition, and ethical considerations.
3. Socio-Cultural and Lifestyle Context
Knowing a patient’s culture, religion, or social situations and the influence of these on their treatment plan is very important, an area where AI still falls short in understanding.
AI is a strong partner, definitely not a substitute. The revolution of oncology resides in the collaboration between humans and AI, where computers are responsible for data and doctors provide care with understanding and empathy.
Why Healthcare Systems Need AI in Oncology Now
Artificial Intelligence is definitely not a futuristic concept anymore; it has become a necessity to address the challenges in cancer care. With increasing cancer incidences, and dwindling healthcare workforce and escalating costs, AI technology is now taking over to provide oncology services that are faster, more accurate, and accessible.
1. Rising Global Cancer Burden
The World Health Organisation has estimated that cancer cases will double from 20 million in 2022 to 35 million in 2050. This alarming rise in cancer has been connected with an unprecedented demand for diagnostic, treatment, and monitoring systems. AI is instrumental in ramping up early detection and making clinical workflows efficient to be able to cope with this increase in numbers.
2. Oncologist Shortage Across Regions
One of the many issues that have challenged the healthcare system in many regions is the shortage of oncologists. A study mentioned that 64% of U.S. counties lack oncologists. Absence of an oncologist in these regions affects timely diagnosis and care. AI tools can help fill the gap by automating triage, diagnostics, and treatment planning, thus, non-specialist providers to do timely interventions.
3. Explosion of Imaging and Genomic Data
The data of modern cancer care from MRIs and CT scans to full-genome sequencing has become a vast body of data conceptualisation where human capability now seems incapable of keeping up at all times. AI is designed for such size, it comes out of intricate sets with datasets to give assistance to the diagnostics of an illness, discovery of mutation and response to the therapy predicted.
4. Rising Costs and Need for Efficiency
Both hospitals and patients undergoing cancer treatment face the challenge of managing the high costs associated with the treatment. AI contributes to reducing the operational cost of running by carrying out duties that are repetitive, reducing the waiting period for diagnosis, and efficiently planning the allocation of resources (for example, radiation therapy planning, follow-up scheduling). In essence, this becomes care that is cost-effective if there is no compromise in quality.
5. Shift Toward Predictive and Personalised Medicine
The future of cancer care is changing from treatment after the fact to predictive and individualised therapy. AI facilitates this transition by detecting high-risk patients at an early stage, customising interventions based on their genetic characteristics, and allowing unobtrusive monitoring. This proactive approach not only enhances life expectancy but also improves overall quality of life.
As cancer care is becoming more and more complicated and the number of patients is increasing all over the world, AI is not only improving oncology but also assisting in its transformation. AI is at the core of constructing a more extendable, just, and data-oriented cancer care system by employing it in various areas such as early diagnosis, targeted treatment, and operational efficiency.
Why Emitrr is the Ideal AI Platform for Oncology Teams
Emitrr, in combination with the innovative AI, private infrastructure, and effortless integration, empowers oncology practices with the new-age capabilities of modern patient engagement. Oncology care requires not only medical precision but also good communication with the patients, which should be efficient as well as empathetic.
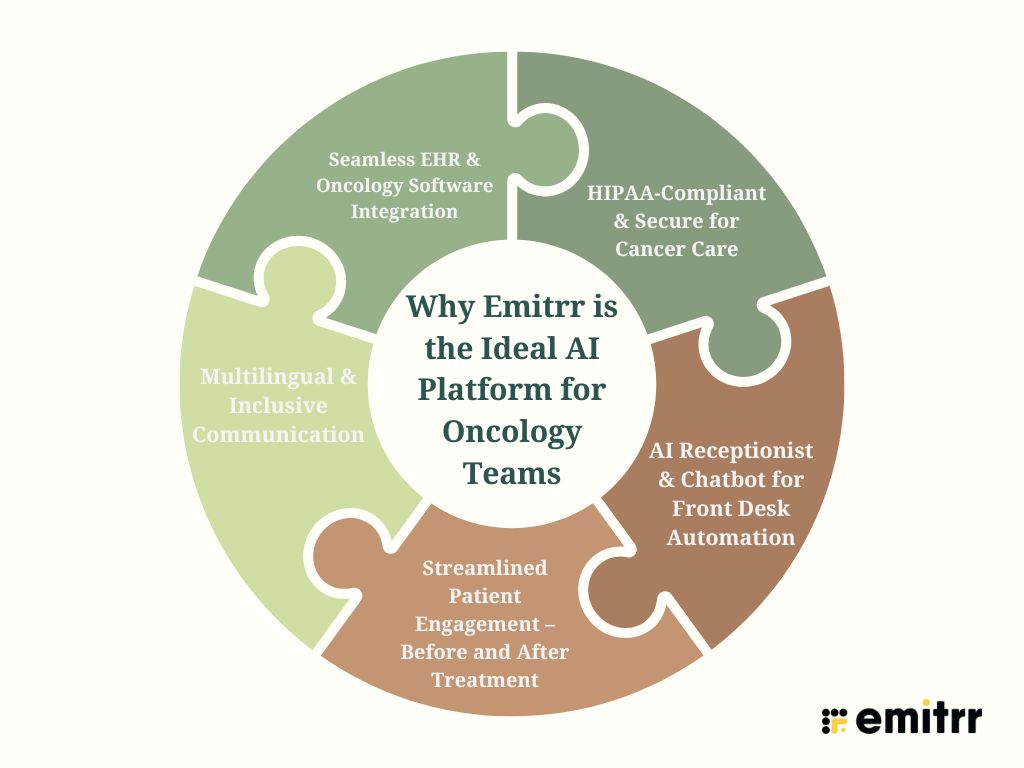
1. HIPAA-Compliant & Secure for Cancer Care
Emitt is a company that sells products that are fully HIPAA compliant, and therefore, they are products that oncologists can use to access patient data without worrying about safety issues. Emitrr enables secure communication with privacy and confidentiality requirements met via AI through secure messaging, voice, and automation.
2. AI Receptionist & Chatbot for Front Desk Automation
Along with the AI receptionist, Emitrr can take care of appointment bookings, changes, reminders, and patient FAQs without human intervention. Hence, the front desk staff will be able to give their full attention to other tasks, the waiting time will be shorter, and cancer patients will have immediate access to reliable information at all times.
3. Streamlined Patient Engagement – Before and After Treatment
Automated pre-treatment instructions sent through Emitrr, along with surgery follow-ups, symptom check-ins, and treatment adherence reminders, not only allow providers to stay connected with patients at every stage of care but also, without carrying out manual outreach.
4. Multilingual & Inclusive Communication
Emitrr can support numerous languages, and then, oncologists can communicate with different patient populations without language being a barrier. As well as voice-to-text, automated translation, and the use of custom messaging templates, these various features allow for uninterrupted access for all and are also inclusive across different regions, as well as literacy levels.
5. Seamless EHR & Oncology Software Integration
Emitrr is a platform that offers a very simple and effortless way of integrating with the electronic health records (EHRs) of oncology that is aimed at setting up communication workflows with AI at the core, which can establish connections directly with the customer records. This not only reduces double entry, keeps the data consolidated, but also ensures seamless care across doctors, nurses, and care coordinators.
Emitrr’s AI Text Enhancement Features
Emitrr has recently launched smart text creation and editing tools designed specifically for oncology teams and front-desk staff who have to communicate with people sensitively. These features are available in Professional Plans and enable teams to respond quickly and more efficiently, as well as in an empathetic way.
- Help Me Write: It creates responses automatically by using prompts (e.g., appointment follow-ups, treatment FAQs, test report delays).
- Enhance:
- Make it Crisp: It clarifies and shortens the messages for understanding and saving time.
- Make it Empathetic: It changes the tone to a softer one and it compassionately adds the feeling of warmth, thus it is most efficient in the oncology sector where there is a lot of talking about sensitive things.
- Suggest a Reply: Robot intelligence understands received messages (e.g., emotional queries or appointment requests) and immediately offers personalised replies.
Emitrr is not only a means of communication, but it is also an AI platform designed for the emotional, operational, and clinical needs of oncology care. Appointment automation, follow-up engagement, and AI-enabled messaging are just a few examples of ways Emitrr helps cancer centres provide compassionate care more efficiently.

Future Trends
Due to increasing challenges in cancer diagnosis and treatment, the application of AI in the oncology field has become extensive. Besides imaging and diagnostics, AI is now helping to change the cancer care industry by high-level modelling, non-invasive screening, and smart treatment planning.
1. AI-Powered Liquid Biopsies
The algorithms of AI offer an interpretation of blood markers such as circulating tumour DNA (ctDNA) and exosomes in a much better way. Therefore, this will allow for continuous, non-invasive, and cost-effective early cancer detection, as well as real-time monitoring of treatment response. To put it differently, the traditional biopsy could thus be unnecessary in certain cases.
2. Digital Twins of Cancer Patients
Digital twins are virtual replicas of a patient’s body that are generated using computer algorithms and real-world data from imaging, genomics, and clinical records. Oncologists can employ these AI-generated models to forecast the reaction of an individual to different treatment options and thus facilitate the personalisation of care before the actual intervention.
3. AI Integration with Immunotherapy
Immunotherapy is efficient for a small group of people alone, whereas AI can come into play to help identify those who will benefit after parsing complicated immunogenomic data. Plus, the application of AI also goes to the point of determining the best dosage, timing, and combinations of immunotherapy drugs.
4. Voice-Enabled Oncology Assistants
Besides other functions, AI-based voice tools can also become a patient’s new furry friend by giving information, playing the role of a doctor to patients, offering emotional support and getting medication instructions. In particular, they are very handy for people with visual impairments, as they serve to facilitate access to care in the cancer journey for patients with low literacy levels or visual impairments.
5. Federated Learning for Secure AI Training
In a decentralised fashion using federated learning, different hospitals can simultaneously train the same AI model to increase medical care without sharing any data. Patient privacy protocols are kept intact by this decentralised approach secure and provides more accurate and diversified models for cancer prognosis.
6. Generative AI for Drug Discovery
One of the most notable applications of generative AI models is in drug design, where the computer not only generates new molecules but also explores drug interactions and accelerates the journey of targeted treatment discoveries. This technology is also a significant tool in cancer research as it helps to come up with personalised cancer drugs at a speed that is far beyond the capabilities of the traditional R&D process.
The advancements are indicative of a move from a reactive approach to cancer treatment to a journey of predictive and precision-based care. The field of oncology, with the help of artificial intelligence-powered tools such as digital twins, liquid biopsy analysis, and generative drug design, is reportedly setting the stage for a new era of research and experimentation, and thus it is going to be one of the most revolutionary decades in the history of medicine.
FAQs
In some instances. AI, which is trained on huge datasets, can find subtle cancer patterns beyond human eyes that are rarely even visible, especially if it is breast, lung, or skin cancer. Google’s AI model, for example, has already demonstrated a higher success rate than some radiologists in recognising breast cancer. These instruments amplify the doctors’ diagnostic accuracy and facilitate a quicker response.
Yes, the FDA has given its green light to several AI-based tools that fall under the category “Software as a Medical Device” for cancer detection. Hence, in such situations, the AI tools are installing the doctor’s capabilities but are not acting as replacements.
AI is not the agent directly responsible for curing cancer. Nonetheless, it contributes a great deal to cancer care by detecting cancer early, making correct diagnoses, tailoring the treatment plan, and rapid drug discovery. AI action covers almost the entire spectrum of oncology, thus resulting in better patient outcomes and more focused therapies.
Certainly not. Near-future AI would, however, take over repetitive work that oncologists do, process enormous amounts of data, and recommend clinical decisions. Still, the oncologists can provide local information, emotional intelligence, and ethical considerations, features that AI cannot copy. The most likely trajectory for the future of cancer care is where there is a partnership between AI and human talents.
Some key issues are:
Bias: The AI models might produce results that are biased in case they have been trained on datasets that are not diverse.
Explainability: The operating principles of most AI are being compared to the actions of a “black box,” thus, their decision-making is difficult to decode.
Privacy: It is of utmost importance to protect the patient data while employing AI-driven systems.
Accountability: It is not clear who will take responsibility if mistakes happen with AI.
Accessibility: High prices and the need for infrastructure may limit the use of AI tools, resulting in situations of unequal care.
Conclusion
Artificial intelligence is revolutionising every phase of cancer care – from early detection and diagnosis to the personalisation of treatment and the monitoring of the patient after the procedure. It facilitates quicker decision making, lessens the workload of the oncologists, and improves the situation by gaining insights from the huge medical datasets.
Although AI boosts accuracy and scalability, thus, it is at its maximum strength when it is used in conjunction with human expertise. The future of cancer treatment is not AI against the doctors but rather AI with the doctors, who are working hand in hand to provide faster, more accurate, and more humane care. If the time has come for your oncology practice to transform, now is the perfect opportunity to take action. Lead the AI revolution with Emitrr first. From HIPAA-compliant communication tools to AI-powered patient engagement and automation, Emitrr helps oncology teams scale smarter, serve better, and stay ahead.

 4.9 (400+
reviews)
4.9 (400+
reviews)