Introduction
Emergency prescription refill requests rarely happen out of nowhere. Most start with a small delay, a missed call, or a refill request that sits unanswered for too long. A patient assumes the refill went through. The pharmacy waits for approval. The practice gets the call when the medication already run out.
Sound familiar?
This guide breaks down what actually qualifies as an emergency prescription refill, why refill requests escalate so often, and how healthcare practices can reduce these situations with better communication.
What Counts as an Emergency Prescription Refill?
Not every early refill qualifies as an emergency refill prescription. Most refills follow strict timing rules.
For non-controlled medications, insurers often allow a refill once about 75 percent of the prior supply is used. A 30-day prescription usually becomes eligible around day 23. Any earlier request often triggers rejection.
Controlled medications follow tighter rules. State laws or pharmacy policy often limit refills to a narrow window. Many pharmacies follow what staff call the 28-day rule. That means at least 28 days must pass before a new 30-day supply becomes available. Some allow only a two-day early refill window.
This is what turns a routine refill into an emergency medication refill!
An emergency refill prescription usually applies when medication runs out due to delays, travel, lost medication, or breakdowns between the practice and pharmacy. The issue today is not the rule itself. The issue is how refill requests move through disconnected systems like the EHR and PMS, without real-time coordination.
Traditional refill paths still rely on phone calls, voicemails, and fax instead of seamless Athenahealth integration. These methods create gaps. A pharmacy sends a fax. A front desk checks it hours later. A provider reviews it at the end of the day inside the EHR. By then, an emergency supply medication request already be waiting at the pharmacy counter.
Common paths patients take during an emergency prescription refill
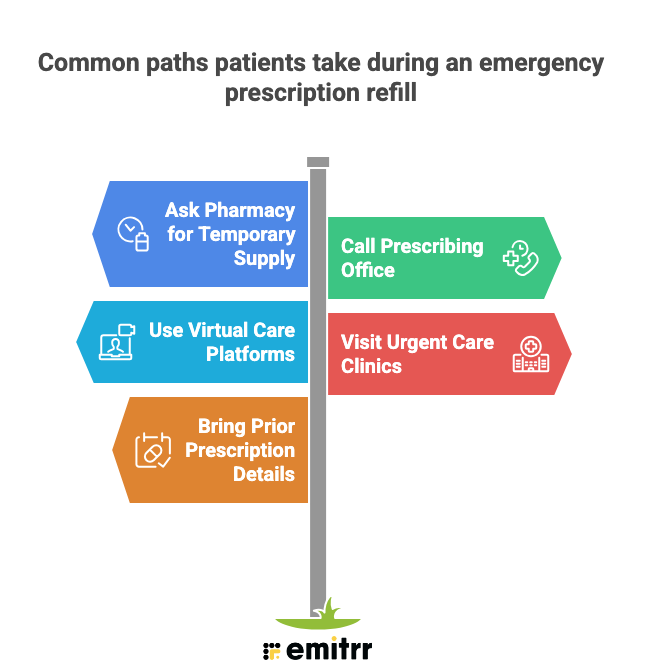
Ask the pharmacy for a temporary supply– Patients often request a short emergency supply of medication to avoid missed doses while approval is pending. This usually applies to maintenance medications and depends on the pharmacy’s discretion.
Call the prescribing office or after-hours line– Many patients contact on-call services after hours, hoping for a quick urgent care prescription refill, which makes it harder for practices to manage after-hours patient messages without overwhelming staff.
Use virtual care platforms– Telehealth visits become a common fallback when patients cannot reach their provider and need an emergency refill prescription the same day.
Visit urgent care clinics– Walk-in or virtual urgent care visits are often used to secure an emergency medication refill when delays feel risky.
Bring prior prescription details– Patients frequently arrive with pill bottles, old labels, or dosage notes to speed up emergency supply medication approval.
These workarounds help patients bridge gaps, but they also highlight how fragmented refill communication creates unnecessary urgency for everyone involved.
Pharmacy-to-Practice Communication Gaps
Most emergency supply medication situations start with silence, not refusal. Refill requests arrive through scattered channels with no shared visibility, so delays go unnoticed until a patient runs out. That breakdown is what turns a routine urgent care prescription refill into an emergency medication refill.
Where things go wrong?
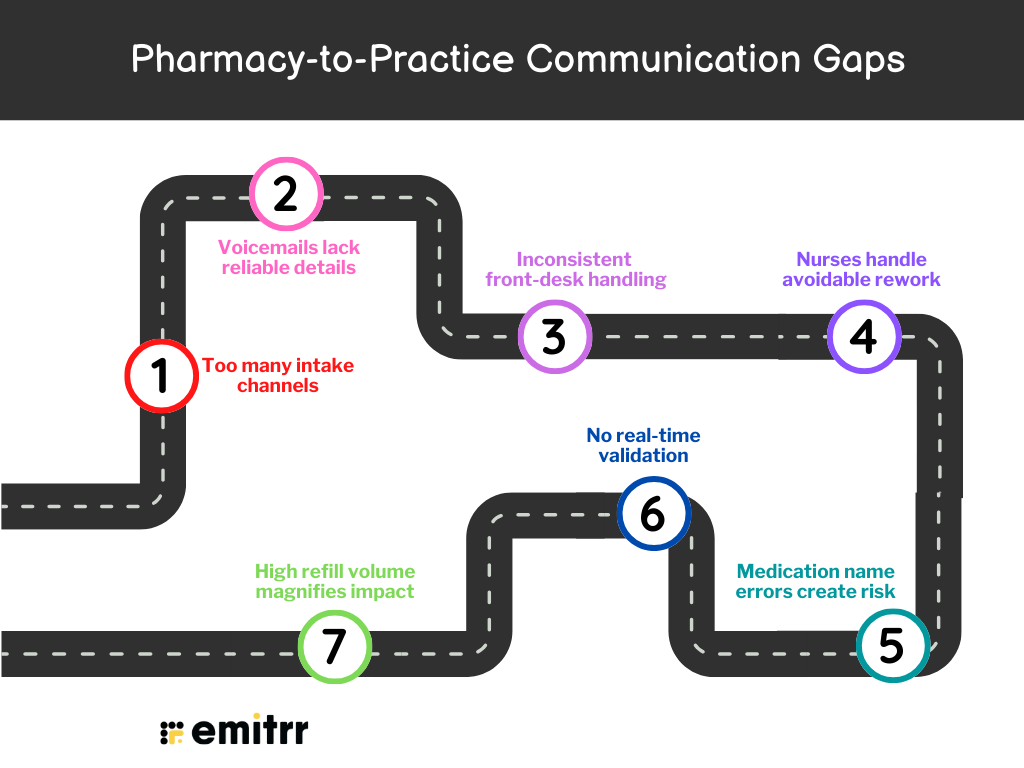
- Too many intake channels: Refill requests come through live calls, voicemails, and patient portals. Each one needs manual review and re-entry. That manual step alone delays emergency refill prescription handling and emergency supply medication approvals.
- Voicemails lack reliable details: Messages often miss patient identifiers, include unclear medication names, or cut off mid-sentence. Staff must call back to clarify, which slows urgent care prescription refill timelines and pushes cases toward emergency medication refill status.
- Inconsistent front-desk handling: Some staff log proper refill requests while others create generic cases. The approach depends on training, not process. This inconsistency adds friction and increases emergency supply medication escalations.
- Nurses handle avoidable rework: When refill requests arrive as cases, nurses re-enter data, check eligibility, and decide routing. This extra work delays emergency refill prescription responses and increases the urgent care prescription refill backlog.
- Medication name errors create risk: Patients often misstate drug names, request medications from outside providers, or ask for discontinued drugs. Each error adds verification steps and slows emergency medication refill decisions.
- No real-time validation: Systems cannot instantly confirm active medications, prescribing provider, or refill eligibility. Without validation, staff must move cautiously, which extends emergency supply medication timelines.
- High refill volume magnifies impact: In practices with high call volume, thousands of refill-related calls compound small delays. Without streamlined workflows, urgent care prescription refill requests overwhelm staff and drive emergency medication refill cases
Check out this video to watch an AI agent handle prescription intake and support faster prescription refill outcomes!
How Emergency Refill Requests Affect Patient Experience
From a patient’s perspective, an emergency refill prescription feels stressful and deeply personal. Medication is not abstract. It ties to daily function, sleep, pain control, or chronic stability. Even a one-day delay can feel dangerous, even when the medication itself is not critical.
Take a common example. A patient finishes their last dose on Sunday night, assuming the refill request left on Friday went through. There was no prescription refill reminder to signal that action was still pending. Monday morning, the pharmacy says approval is still on hold. The practice has no record of urgency. That gap instantly turns into an emergency medication refill situation.
Patients respond the only way they know how. They call the front desk repeatedly. They walk into the pharmacy to ask again. Some send portal messages while still calling. Others post a negative review after hours of silence. None of this behavior starts from impatience. It starts from uncertainty.
When urgent care prescription refill requests lack clear updates, trust drops fast. Patients do not separate insurance timing rules from practice workflow or pharmacy delays. They do not see fax queues or voicemail backlogs. They only see one thing. Medication runs out.
Another frequent scenario involves controlled medications. A patient requests a refill one day too early. The request gets rejected silently. With no guidance toward a telehealth prescription refill, the patient waits without explanation. By the time staff follow up, the patient already feels ignored, even though the rule caused the delay.
This communication gap, not the refill rule itself, is what damages the patient experience.
What Patients Experience vs What Practices See
| Patient experience | What’s happening behind the scenes |
| “No one is responding to my refill request” | The request sits in voicemail, fax, or an untriaged inbox |
| Multiple calls in one day | Staff waits on provider review or clarification |
| Pharmacy says “still pending” | No shared visibility between pharmacy and practice |
| Feels like an emergency medication refill | Timing rules or missed handoffs delay approval |
| Loss of trust in the practice | Patients feel ignored when refill requests stall inside manual workflows |
Preventing Refill Emergencies Through Better Practice Communication
Emergency refill requests do not disappear on their own. Practices that reduce them take deliberate steps to fix patient communication gaps before medication runs out.
What practices should do first?
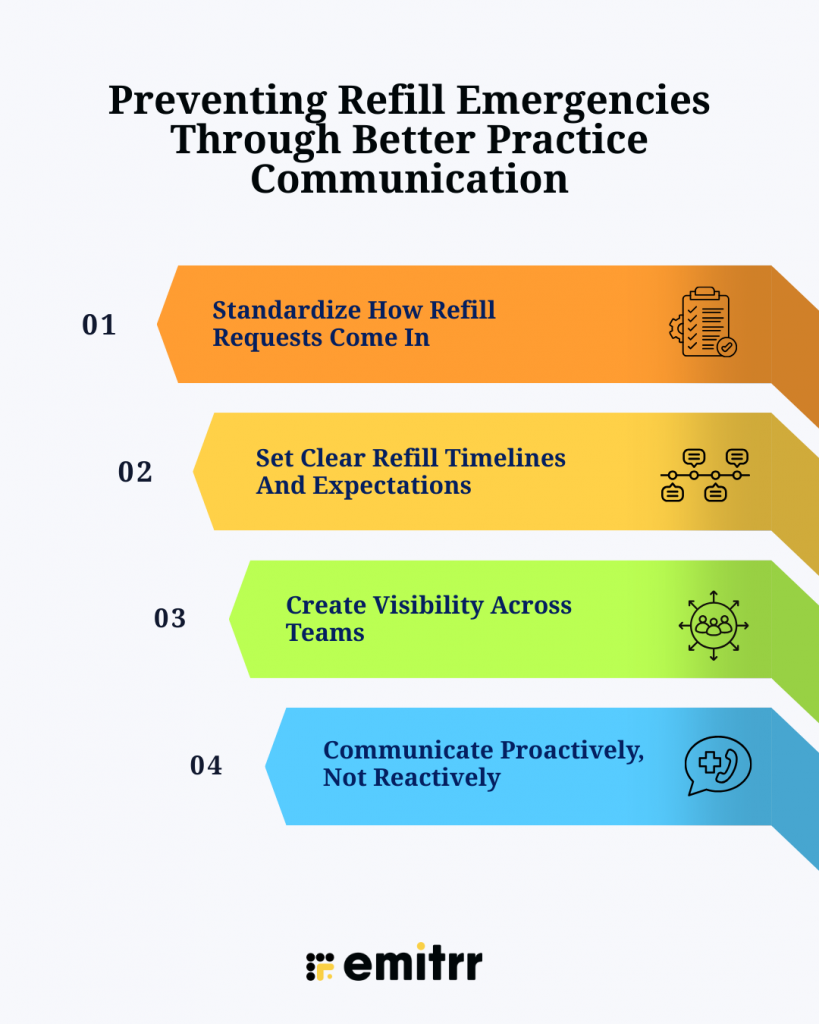
- Standardize How Refill Requests Come In
Refill requests should flow through one clear, structured channel. When phone calls, voicemails, and Athenahealth Patient Portal messages all compete for attention, emergency prescription refill situations increase.
- Set Clear Refill Timelines And Expectations
Patients need to know when to request refills and what happens next. Clear timelines reduce last-minute urgent care prescription refill pressure and emergency supply medication requests.
- Create Visibility Across Teams
Front desk, nurses, and providers should see the same refill request status. When requests disappear between roles, emergency medication refill cases rise.
- Communicate Proactively, Not Reactively
Waiting until medication runs out forces urgency. Proactive outreach prevents emergency refill prescription scenarios entirely.
Want to see how practices text patients directly from Athenahealth to prevent refill emergencies?
Watch this video to see how Emitrr enables real-time, two-way patient messaging without leaving the Athenahealth workflow –
Using Emitrr AI to Reduce Emergency Prescription Refill Volume
A large share of prescription refill requests follow predictable patterns and do not need staff-led intake. Patients share the same information every time. Name. Date of birth. Medication. Dose. Pharmacy. When this intake stays manual, delays stack up, and emergency medication refill situations become routine.
Practices that automate this first layer see a measurable drop in refill chaos. Emitrr customers reduce front-desk refill call volume by up to 40 percent while keeping provider review exactly the same. The difference is structure, not shortcuts.
Instead of relying on voicemails, phone tags, or manual message reading, practices use Emitrr to standardize refill intake before staff ever touch the request.
Enter the AI agent: the future of refill intake
Basic SMS helps, but it still requires staff to read, interpret, and re-enter information. A HIPAA-compliant AI agent goes further. It acts as a digital team member that handles refill intake consistently, without fatigue or variation.
When a practice deploys Emitrr’s AI agent, it takes over the intake portion of the prescription refill request process entirely.
1. Consistent data capture every time
The AI gathers patient name, date of birth, medication, dosage, and preferred pharmacy in a guided interaction. No skipped fields. No guessing.
2. Structured cases, not sticky notes
With AI and EHR integration, refill requests arrive as structured cases instead of scattered messages that require manual context rebuilding.
3. Full visibility without staff interruption
The AI answers calls directly, records the conversation, and provides a clear summary or full transcript. Staff review instead of listening to voicemails.
Match-first efficiency that prevents emergencies
Once the AI captures the refill request, it compares the information against existing patient and medication data.
- If the details match clinic rules and active prescriptions, the request moves forward without delay.
- If something does not align, such as an out-of-refill medication or a mismatch in drug details, the AI flags it and creates an escalation case for staff review.
This match-and-route approach prevents unsafe approvals while avoiding unnecessary back-and-forth. Most importantly, it stops valid refill requests from stalling long enough to become emergency prescription refill situations.
Centralized AI intake replaces scattered refill channels
Emergency refill prescription issues often begin when requests arrive through too many paths. Phone calls. Voicemails. Portal messages. Each one requires staff interpretation.
Emitrr’s healthcare AI agent becomes the first point of contact for emergency prescription refill and routine refill requests through voice or SMS. Every request enters through one standardized flow. Refill intent stays clear from the first interaction, which prevents misrouting and missed urgency.
This alone reduces emergency supply medication escalations caused by overlooked messages.
Here’s a short video about Emitrr’s AI Voice Agent handling refill calls end-to-end, capturing details accurately, and preventing emergency prescription refill delays before staff ever step in –
Structured refill intake with no missing details
Incomplete information fuels urgent care prescription refill delays. Emitrr’s AI agent collects refill details through a guided, conversational interaction.
The AI captures patient identifiers, medication name, dosage, frequency, and preferred pharmacy. If something sounds unclear, it asks again immediately. Each request produces a structured summary, a full transcript, and a call recording.
Refill requests arrive complete the first time. No callbacks. No guesswork. Fewer emergency medication refill follow-ups.
Automatic case creation without manual rework
Once intake is complete, Emitrr automatically creates a case inside the EHR. All patient-provided details, the AI summary, transcript, and recording are attached to that case.
Staff no longer listen to voicemails or retype information. They review instead of reconstructing context. This removes one of the biggest drivers of emergency refill prescription delays.
One consistent refill logic, every time
In manual workflows, refill handling depends on who takes the call. Training gaps create inconsistency.
Emitrr’s AI agent follows one refill intake logic across all requests. Same questions. Same structure. Same checkpoints. Business hours or after hours, the intake stays consistent.
This consistency prevents refill requests from slipping into emergency medication refill status due to process variation.
Match-based routing protects safety without slowing care
Patients often mispronounce medication names, request discontinued drugs, or ask for medications prescribed elsewhere. Emitrr’s AI does not approve refills.
If information aligns with existing records and clinic rules, the request moves forward. If something does not match, the AI flags it for review. This protects safety while keeping valid emergency prescription refill requests moving.
AI handles intake at scale, staff handles decisions
Emitrr’s AI agent manages refill intake around the clock. Nights, weekends, and holidays included.
By morning, staff see organized refill cases instead of voicemail backlogs. Nothing sits unseen. Nothing escalates simply because offices were closed. Emergency supply medication requests drop because intake no longer pauses after hours.
Frequently Asked Questions
In some cases, a pharmacy may offer a limited emergency supply of medication based on state rules, medication type, and the pharmacist’s discretion. This usually covers only short durations.
When refills expire, the pharmacy must contact the prescribing provider. Delays here often trigger emergency medication refill situations.
Some prescriptions allow renewal without a visit, but approval still requires provider review. Communication speed matters.
Pharmacist authority varies by state and medication class. Controlled drugs usually require provider authorization.
Costs depend on insurance, drug type, and refill timing. Emergency refill prescription scenarios may affect coverage.
Key Takeaways for Healthcare Practices
- Most emergency prescription refill issues start with communication gaps: Emergency prescription refill situations usually happen due to missed messages, delayed intake, or unclear workflows, not because patients act late.
- Manual refill intake increases urgency and workload: Phone calls, voicemails, and portal messages slow response time. These delays turn routine requests into urgent care prescription refill situations and emergency supply medication requests.
- Incomplete information fuels refill chaos: Missing details like medication name or pharmacy force callbacks and rework. This increases emergency medication refill volume and frustrates both staff and patients.
- After-hours silence creates unnecessary emergencies: Refill requests that arrive on nights or weekends often sit untouched. By the time staff responds, the request has already become an emergency prescription refill.
- Standardized intake prevents last-minute escalation: When every refill request follows the same structured path, fewer cases escalate into emergency medication refill scenarios.
- Automation reduces emergency refill volume without clinical risk: AI-led intake handles repetitive data collection while staff focus on review and decisions. This lowers urgent care prescription refill pressure without changing provider oversight.

 4.9 (400+
reviews)
4.9 (400+
reviews)