Introduction to AI Medical Coding
Let’s be real, medical coding isn’t for the faint of heart. With frequently updated guidelines, unstructured documentation, and pressure to code accurately and quickly, it’s becoming tough for medical coders.
The growing complexity of medical notes and the sheer volume of codes to pick from can make even the most experienced coder feel overwhelmed. On top of that, incomplete physician documentation, contact updates, and inconsistencies in the system only add to errors, claim denials, and lost revenue.
But the good news is that AI in healthcare is stepping in to help. AI and smart coding tools are transforming the way medical coders work. They make tedious processes faster, more accurate, and far less frustrating.
Today, we are breaking down the major challenges medical coders face today along with how AI can lend a helping hand.
What is Medical Coding?
Medical coding is the conversion of healthcare diagnoses, medical services, treatments, and equipment into universal medical alphanumeric codes. These codes are derived from medical record documentation, including transcription of physicians’ notes, radiologic results, etc.
Medical coding is like translating a doctor’s notes into a special language that computers and insurance companies can understand. Medical coding professionals then apply these codes accurately during medical billing. This includes abstracting the information from data, assigning the correct codes, and preparing a claim to be paid by insurance carriers.
So, medical coding takes place every time you pay a visit to a healthcare professional. As the medical providers review your query and medical history, they make an expert assessment of the issue, how to treat and document it all. This documentation is not only the patient’s ongoing record, but it’s also how the healthcare provider gets paid.
Challenges Faced by Medical Coders
Medical coding may seem like a behind-the-scenes job, but it’s absolutely essential to the healthcare system. It is a dynamic and complicated process that requires ultimate focus in translating strategies, medical diagnoses, and treatments into standardized codes.
But this is not all, the frequent changes in coding guidelines and documentation variations can cause multiple challenges for medical coders. Let’s look at the most critical challenges and understand why they occur.
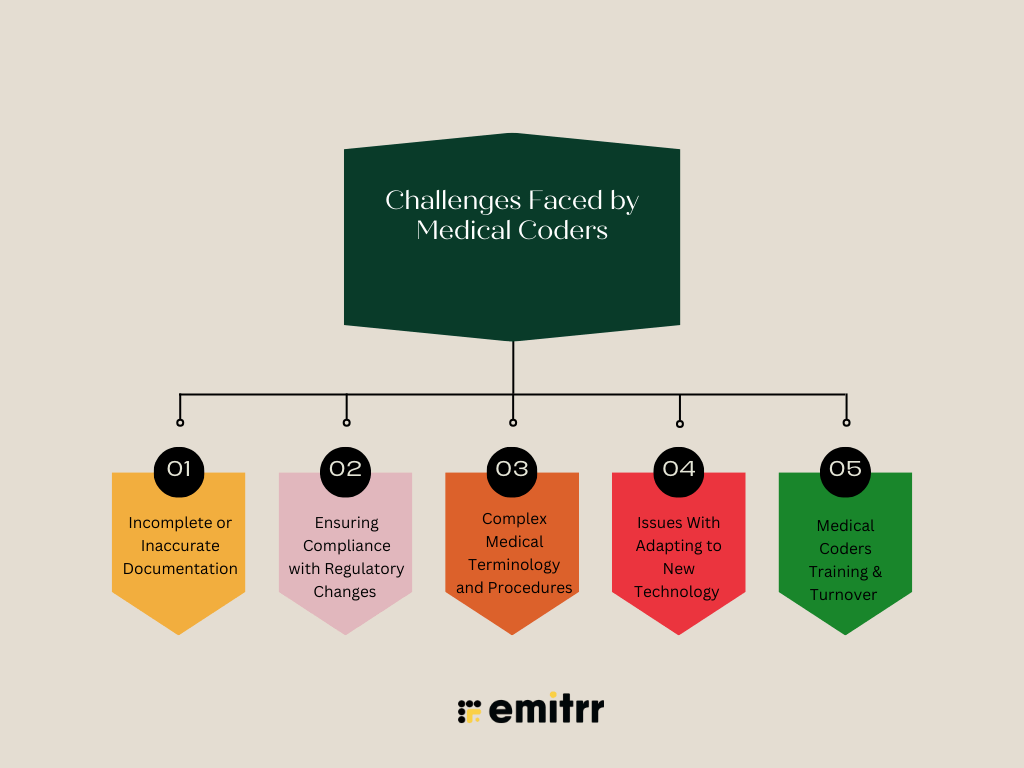
Incomplete or Inaccurate Documentation
Medical coders are highly dependent on physician notes and clinical summaries to do their job. When doctors rush through documentation or use inconsistent terminology, it can result in undercoding, overcoding, or claim denials. In fact, coding errors account for nearly 15–25% of all claim denials, impacting revenue cycles and reimbursement rates.
The lack of structured documentation, insufficient training, and poor record maintenance can cause communication gaps between healthcare providers and medical coders, which further adds to this challenge. While accurate coding is significant for medical reimbursement and compliance, working fast can cause quality issues for coders.
This poor documentation not only affects medical coders but also affects patient records, impacting clinical decision-making and the overall healthcare system.
Ensuring Compliance with Regulatory Changes
The medical billing and coding industry is changing constantly. With the introduction of new regulations, coding guidelines, and frequent updates, medical coders struggle to stay updated with the regular changes.
These changes in coding guidelines, payer policies, and billing requirements impact how healthcare providers document and report services. This makes compliance a big challenge.
Medical coding regulatory updates are introduced to showcase advancements in medical practices. This includes billing accuracy and patient engagement solutions.
However, adapting to these regulatory updates demands awareness, continuous education, and procedural adjustments. Without a proper training system in place, coders struggle to implement and use new guidelines properly.
The bigger concern is that failing to stay updated with regulatory changes can lead to claim denials, non-compliance, and financial discrepancies. Moreover, using outdated coding practices results in revenue loss and stricter observations from auditors.
Complex Medical Terminology and Procedures
The medical coder’s role involves translating complex medical terminology and practices into standardized codes. These codes are used for billing and documentation. This requires a thorough understanding of medical language, including anatomy, physiology, and other medical specialties.
This challenge comes from the massive medical vocabulary, including terms derived from Latin and Greek, and numerous abbreviations and acronyms. Without a strong understanding of medical terms, coders can misinterpret documentation, leading to incorrect code assignments. This may result in claim denial, compliance issues, and potential legal issues.
Different medical specialties have different terminologies. For example, cardiology and neurology have unique terms, which require coders to be familiar with a vast number of terms to ensure accurate coding across various fields.
Without a solid grasp of medical terms, coders may misinterpret documentation, leading to incorrect code assignments. This can result in claim denials, compliance issues, and potential legal consequences.
Issues With Adapting to New Technology
New technology integration in medical coding can be a blessing for medical coders, but only if used properly. Many healthcare providers still rely on outdated software that doesn’t fit well with the updated healthcare system. To add to the challenge, some medical coders might not be fully trained to use these advanced coding tools.
The bigger challenge is to get these platforms to communicate with each other. When medical systems don’t connect properly, it leads to discrepancies in documentation, inaccurate coding, and delayed billing. For medical coders, there is always a hesitation or resistance to new technology, which can hold back improvements.
Thus, without proper technology integration, there can be delays in managing patient records and the overall coding workflow.
Medical Coders Training & Turnover
When highly qualified medical coders leave the system, it disrupts the whole medical coding workflow. New hires in medical coding often need time to learn new practices and settle down in the system. Without any proper training, this can lead to inconsistencies in documentation and coding workflow.
With high staff turnover, teams are often working with different skill levels, increasing the chance of errors. Training new coders repetitively can increase pressure on time and physical burnout. With no particular definitive training program in place, medical coders can get confused, leading to inaccuracies.
Thus, medical coders require continuous training to keep up with the evolving coding standards, further pushing staff and budgets. Without proper training, coding teams and healthcare organizations face slower coding, more claim denials, and greater compliance risks.
Understanding AI in Medical Coding
Medical coding plays a significant role in the healthcare industry by ensuring that healthcare professionals receive correct reimbursement for their services. Their main role is to ensure that healthcare providers are paid correctly and on time for the services they deliver.
However, with the growing complexity of healthcare data and coding requirements, medical coding challenges are on the rise. This is where Artificial Intelligence (AI) comes into play in medical coding. AI in medical coding is assisting healthcare professionals by automating repetitive tasks, spotting errors, and improving coding workflow accuracy.
As medical coding continues to evolve, healthcare and RCM (Revenue Cycle Management) leaders are turning to AI to simplify the process and streamline their operations. AI makes the process more efficient for coders. Within just a few clicks, coders can receive accurate suggestions for AI medical coding, saving them time and reducing errors.
Although AI isn’t here to replace coders, it’s here to support them, AI allows medical coders to focus on what they do best. This includes applying human judgment to complex cases, resolving discrepancies, and ensuring all codes meet current standards and regulations.

How is AI in Medical Coding Solving Challenges?
As we discussed the role of AI in medical coding in the previous section, let’s look at how AI assists in solving medical coding challenges for medical coders.
Smart Data Extraction for Accurate Documentation
Rushed documentation, uneven terminology, and missing bits are common issues that lead to undercoding, overcoding, and claim denials. This challenge often stems from a lack of structured documentation practices, limited training, and poor communication between healthcare providers and coders.
However, medical billing AI tools bridge these gaps and improve documentation quality in multiple ways.
- Real-time documentation: AI in medical coding can help physicians during patient engagement by offering real-time prompts, reminders, and structured templates to make sure all important details are recorded.
- Natural Language Processing (NLP): AI with NLP capabilities can discover unstructured data and convert it to structured, standardized formats that are easier for coders to understand and code accurately.
- Identify Missing information: Medical billing AI can review records and flag any conflicting entries, aiming for immediate follow-up before the coders even begin their work.
- Reducing Time Pressure: By streamlining documentation and reducing manual review, AI agents free up coders’ time. This allows them to focus more on accuracy and compliance rather than rushing through poorly written records.
Notably, some studies have reported a 19% to 92% decrease in documentation time with AI medical coding software, highlighting significant efficiency gains
Built-In Compliance Checks
Medical coding is governed by dynamic regulations and strict coding standards. Staying updated with these changing regulations can be overwhelming at times. But not with AI. AI in medical coding steps in as a powerful assistant with built-in compliance checks to help coders and healthcare organizations stay compliant with ease and accuracy.
Here’s how AI supports compliance checks:
- Real-time monitoring of regulatory changes: AI medical coding software regularly scans regulatory sources like CMS, ICD, and CPT updates to detect any new changes. Using NLP, AI agents can crack complex policy language and highlight what coders need to know, right when they need it.
- Predictive Risk Analysis: Machine learning models analyze past coding data to spot any trends and predict compliance issues that might arise. This helps organizations proactively adjust their processes or offer targeted training to medical coders.
- Automated compliance checks: A medical coding software performs real-time audits during the coding process. It flags entries that don’t align with current regulations or payer rules. This helps minimize the risk of denials and non-compliance penalties.
- Streamlined reporting and documentation: AI can generate detailed compliance reports to create a clear audit trail for internal use or external inspection. Thus, saving a lot of time and the risk of documentation errors.
The great part is that implementing AI in medical coding has shown a reduction in errors and saved time for medical professionals, reviewing electronic health records.
Advanced Language Processing for Complex Terminology
Medical coders often struggle with complex medical terms and multifaceted procedures, leading to coding errors. AI technologies are transforming this by enhancing accuracy and efficiency.
- Understanding complex medical language: Medical coding automation tools, particularly those using Natural Language Processing (NLP). It can interpret difficult medical terminology and scattered clinical notes. This capability allows AI to extract relevant information and suggest correct codes, minimizing the risk of errors.
- Automating code assignment for complex cases: AI can process multi-procedure cases and complex diagnoses easily. This automation speeds up the coding process and enhances consistency.
- Supporting Medical coders with strategic thinking: AI software used for medical billing and coding serves as a decision-support tool, assisting human medical coders by eliminating discrepancies and suggesting corrections.
Integrating New Technology with AI
Adapting to new technology in medical coding can be a major challenge for medical coders. But AI software used for medical billing and coding make things easier. Did you know that, integration of AI in healthcare reduced around 20% of physicians’ time in administrative tasks.
AI helps in streamlining the learning process, automating complex and dynamic tasks, and providing real-time support. This ultimately makes the shift to new coding systems and updates smoother for medical coders.
Here are some key ways AI medical coding software helps address the challenge of adapting to new technology in medical coding:
- Simplifying complex systems: AI-powered tools often feature user-friendly interfaces that streamline the coding process, reducing the learning curve associated with new technologies.
- Automating routine tasks: By handling repetitive and time-consuming tasks, AI allows coders to focus on more complex tasks, making the adoption of new systems seemingly easier.
- Providing continuous learning opportunities: AI offers real-time feedback and suggestions as an on-the-job training tool that helps medical coders adapt to new coding standards and technologies.
- Supporting workflow integration: AI can be integrated into existing workflows, reducing any hiccups and facilitating a smoother transition to new technological platforms.
Enhancing Training Processes
As discussed in the challenges section, high turnover and continuous need for training in medical coding departments can disrupt the overall coding workflow. According to a recent survey, 79% of healthcare professionals think robotics and AI will significantly transform the healthcare industry.
- Accelerated onboarding with continuous learning: AI-driven training platforms offer interactive and personalized learning experiences. This enables coders to grasp complex coding systems more easily. It also reduces the learning curve and supports continuous skill development.
- Real-time feedback and error correction: AI medical coding software offers real-time feedback on coding decisions for medical coders. This guidance creates a supportive learning environment and enhances coder confidence.
- Reduces workload stress: By automating repetitive tasks, AI reduces the administrative burden on medical coders. It allows them to focus on more complex and dynamic cases. This shift can lead to greater job satisfaction and lower turnover rates.
- Standardized training process: Medical billing automation tools helps in designing standard training protocols, ensuring all coders receive the same level of instructions and support. This unity across the organization maintains coding quality and reduces errors in coding practices.
- Proactive Analytics for Workforce Planning: AI can analyze workforce data to predict potential turnover trends, allowing organizations to proactively address issues and implement retention strategies.

How to Maximize the Benefits of Automated Medical Coding?
The best potential of AI in medical coding is not just in its implementation but in how it is strategically used and managed by healthcare professionals. Let’s see how you can enhance the benefits of AI in medical coding and produce the best results:
Integrate AI with Human Expertise
Medical billing automation AI quickly examines massive data, auto-suggests codes, and spots inconsistencies in medical documentation. However, it lacks the deep knowledge that human coders bring to the table. This is a concern in complex and dynamic cases where medical context and clinical judgment are required.
One thing to note is that AI is here to support humans and not to replace them. So, medical coders must use AI coupled with their expertise in the area.
- Use AI as a first-level reviewer or “coding assistant” to handle high-volume, low-profile cases
- Let the certified coders focus on reviewing AI-suggested codes, making final edits, and handling outlier cases
- Train medical teams to collaborate with healthcare coding and billing AI tools rather than seeing themselves as replacements
Regularly Train and Update Healthcare Coding and Billing AI Models
AI algorithms are only as good as the data and rules they are trained on. Medical coding is not only complex but also dynamic. IDC, CPT, and HCPCS codes are revised annually, and payer policies often change. If healthcare coding and billing AI models are not updated, they risk applying outdated codes, causing compliance issues.
Continuous learning and retraining of medical coding AI models ensure their relevance and reliability in a constantly changing field.
- Team up with vendors or data scientists to update AI models as per CMS, AMA, and ICD code set changes
- Train models with the updated clinical data, payer feedback, and real-world case scenarios
- Perform ongoing validation to ensure accuracy and compliance with healthcare coding standards
Ensure Data Quality and Consistency
AI models rely heavily on the quality of input they receive. If there are inconsistent formats, poor documentation, or incomplete records, it will definitely affect its performance, resulting in inaccurate coding. And worse, this poor-quality data can train AI healthcare coding and billing systems to repeat and scale these errors.
- Implement strict data validation checks to make sure only clean and structured records are used
- Maintain uniform documentation standards across all departments to support consistent data input
- Monitor EHR systems for formatting discrepancies that might confuse AI medical billing software.
Prioritize Data Security and Patient Privacy
When AI is handling massive volumes of sensitive patient data, protecting that data is non-negotiable. The risk of breaches, misuse, or non-compliance with regulations like HIPAA guidelines or GDPR can result in legal consequences and loss of trust. A data breach like this can lead to compromised patient confidentiality and regulatory penalties.
- Make sure encryption protocols, role-based access, and audit trails are a part of your AI medical billing software.
- Select AI vendors perform HIPAA compliance audits and prioritize secure cloud infrastructure
- Keep testing for vulnerabilities and establish an incident response plan
Monitor Performance for Optimization
To get satisfying results, it’s important to treat medical billing AI like a living system that requires ongoing performance monitoring, feedback, and optimization. AI must be evaluated on both technical and business outcomes. AI medical billing software models may drift in performance over time, so continuous monitoring is significant for accuracy.
- Set KPIs in place, such as coding accuracy rates, time saved per case, or claim denial reductions
- Use dashboards to track real-time performance and minimize any pain points
- Strong feedback from coders to polish AI workflows and identify new training needs
Why Emitrr is the Best AI Medical Coding Software?
When it comes to AI medical coding, Emitrr doesn’t just keep up, it leads the way. Emitrr is designed specifically for healthcare professionals, which makes coding smoother, faster, and a whole lot less stressful.
Here’s why it’s a favorite among medical practices:
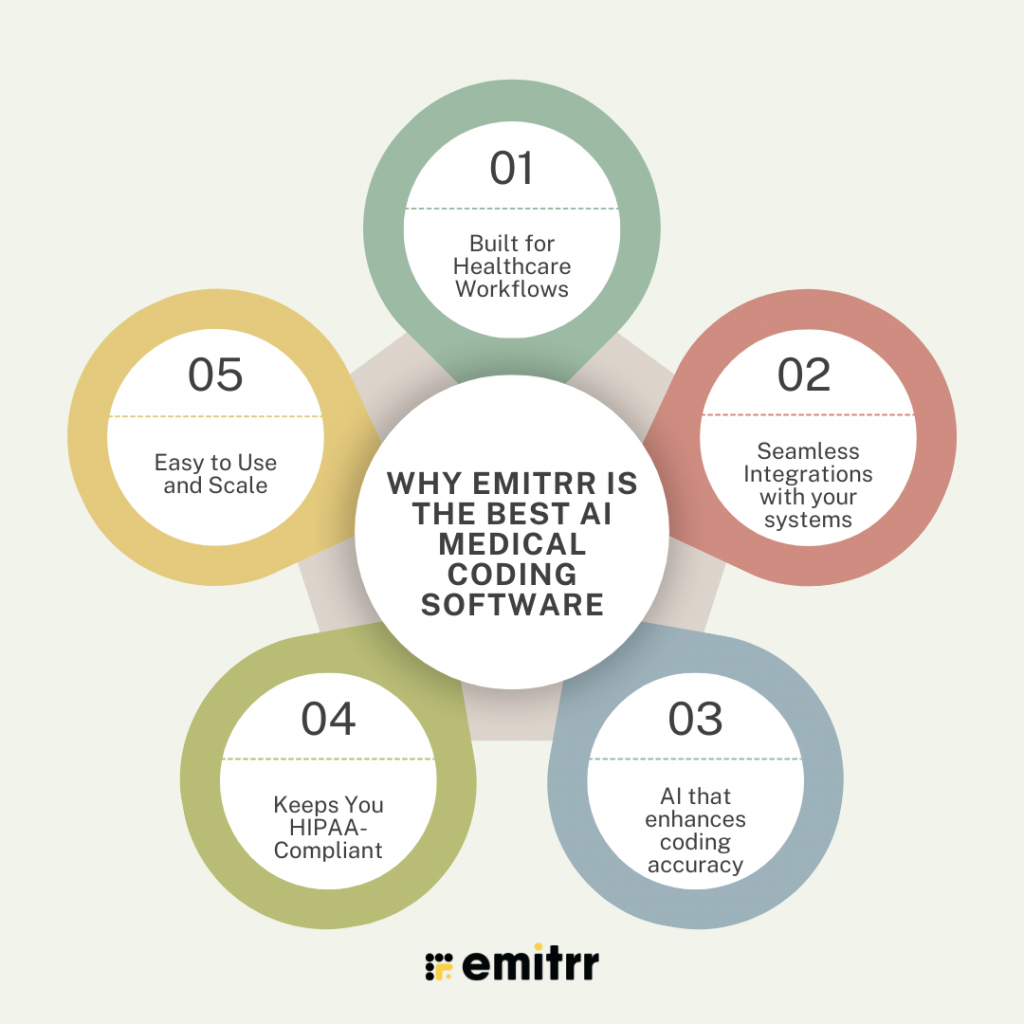
Medical Coding AI Built for Healthcare Workflows
Emitrr isn’t your basic automation tool, it’s the best CRM for healthcare. From automating repetitive admin tasks to streamlining patient interaction, everything is designed to lighten the load on your staff so they can focus on what really matters. This makes it the best AI for medical coding.
Seamless Integrations with your systems
No more juggling between platforms. Emitrr medical coding AI works hand-in-hand with popular EHRs, EMRs, and billing software ensuring accurate real-time syncing of data. This means fewer errors, smoother claims, and better coordination across your team.
Medical Coding AI that enhances coding accuracy
Emitrr uses AI to suggest accurate codes based on your documentation, flag potential errors, and even recognize patterns over time. It’s like having a super-smart assistant who never gets tired.
Keeps You HIPAA-Compliant
Worried about data privacy? Emitrr medical coding AI has got your back. It follows strict HIPAA guidelines to ensure patient feedback stays secure, so you can automate with confidence and peace of mind.
Easy to Use and Scale
You don’t need to be tech-savvy to get started with Emitrr. Its intuitive interface makes it easy for teams to adapt quickly. And as your practice grows, Emitrr grows with you, no disruptions, no headaches.

FAQs
AI scans medical records for context, highlights inconsistencies, and offers the most accurate codes. This reduces human error, claim denials, and improves overall coding precision.
AI uses machine learning to study patterns in complex clinical data and identify applicable codes. It supports coders by narrowing choices and flagging critical details in multi-layered cases.
NLP helps AI read and interpret unstructured text like physician notes and discharge summaries. It extracts key medical terms and turns them into structured, codable data.
AI tools integrate with EHRs and billing systems through APIs or direct sync. This enables real-time documentation analysis without disrupting existing workflows.
This happens with automating repetitive tasks like code selection and error detection, AI lightens coders’ workload. This helps them focus on critical tasks and reduces mental fatigue.
Tools like Emitrr, Optum360, MediCodio, and FinThrive use AI to assist with coding, accuracy, and revenue cycle management. Each supports different parts of the workflow.
No, medical coding is unlikely to be done completely by AI. While artificial intelligence in medical coding is helping improve efficiency, reduce errors, etc., it is unlikely to replace human coders entirely.
AI in medical billing and coding comes with several risks in regards with privacy, accuracy, ethical concerns, incomplete or biased information, and more. While AI can certainly improve efficiency, it has its own set of drawbacks that must be taken into account. Issues such as potential data breaches, lack of nuanced human judgment, bias, etc., are things that you must consider.
Automated medical coding tools like Emitrr, MediCodio, Optum360, etc., are some of the best automated medical billing tools. All of these tools help with different aspects of medical billing, you can choose the one that best fits your needs.
Automated medical billing and coding have already become a reality. Healthcare businesses are increasingly incorporating artificial intelligence in medical coding and billing-related processes for simplifying workflows, reducing errors in documentation, generating medical billing codes, and more. However, it has not replaced human medical coders entirely and is not likely to.
Conclusion
AI is transforming medical coding for medical coders. And yes, it’s not just assisting in the usual day-to-day tasks; it’s about taking over the burden of medical coders, channeling it towards productive and accurate results.
With this in mind, Emitrr offers healthcare-specific AI solutions that not only boost coding accuracy but also ease the overhead pressures of medical teams.
Curious how this looks in action? Try Emitrr for yourself. Schedule a demo and explore how AI can enhance your coding game while keeping patient care in focus.

 4.9 (400+
reviews)
4.9 (400+
reviews)